Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 19 April 2024, 11:34 PM
Nutrition: 9. Managing Acute Malnutrition
Study Session 9 Managing Acute Malnutrition
Introduction
While monitoring the growth of children and promoting good feeding, caring and health seeking behaviours, you may find children who need intervention because of acute malnutrition.
You need to know how to identify acute malnutrition and how to differentiate between severe acute malnutrition, and moderate acute malnutrition. In this session, you will apply your knowledge of nutritional assessment to decide whether children are acutely malnourished or not. The study session will teach you how to make further use of anthropometric measurements like MUAC (mid-upper arm circumference), oedema, weight and height which you learned about in Study Session 5. Finally, you will learn the principles of management of people with moderate acute malnutrition. You will look at the management of people with severe acute malnutrition in Study Session 10.
Learning Outcomes for Study Session 9
When you have studied this session, you should be able to:
9.1 Define and use correctly use all key words printed in bold. (SAQ 9.1)
9.2 Explain the use of anthropometric measurements for identification of acute malnutrition. (SAQ 9.2)
9.3 Explain how to interpret anthropometric measurements. (SAQ 9.2)
9.4 Describe how to care for children with moderate acute malnutrition (MAM). (SAQs 9.1 and 9.3)
9.5 List the components of, and be able to plan for, Enhanced Outreach Strategy/Child Health Days (EOS/CHD). (SAQ 9.4)
9.6 Explain the main features of service organisation for EOS/CHD. (SAQ 9.4)
9.1 Anthropometric criteria for defining severe and moderate acute malnutrition
Table 9.1 overleaf shows the criteria (indicators) you need to use to decide the level of acute malnutrition. When the nutritional status of a child deteriorates in a relatively short period of time, the child can be said to have acute malnutrition. As you saw in Study Session 5, weight-for-height, MUAC and oedema are used to decide if someone is acutely malnourished or not. Oedema in children almost always signifies the presence of severe acute malnutrition. However, when using MUAC and weight-for height you need to use ‘cut-offs’ in order to determine whether a child has moderate acute malnutrition, severe acute malnutrition or no acute malnutrition.
| Indicator | Severe acute malnutrition | Moderate acute malnutrition | No acute malnutrition |
|---|---|---|---|
| Children (6 months up to 18 years) | |||
| W/H (weight for height) | Less than 70% of norm | 70-79.99% | More than 80% |
| Oedema (bilateral and pitting | Present | Absent | Absent |
| MUAC (cm) | Less than 11 cm | 11-11.99 cm | More than 12 cm |
| Adults (older than 18 years) | |||
| BMI | Less than 16 | Between 16-16.99 | 18.5-24.99 |
| Oedema | Present | Absent | Absent |
| MUAC (cm) | Less than 17 cm or Less than 18 with recent weight loss or chronic illness | 17-21 cm or 18-21 cm depending on presence of recent weight loss or chronic illness | No weight loss |
As indicated in the table, there are different indicators for severe acute malnutrition and moderate acute malnutrition depending on whether you are measuring an adult or a child. If you look in the column ‘severe acute malnutrition’ (SAM) you will see that if a child’s weight/height measurement is less than 70% of the normal range for his age (which can also be written as
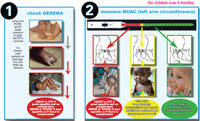
The presence of one criterion is sufficient to categorise a patient as malnourished. If there is any one indicator from the severe acute malnutrition column, then the child or adult is classified as severely malnourished. If there is no indicator in the severe column, and there is at least one indicator in the moderate acute malnutrition column, then the child or adult is classified as moderately malnourished. If none of the indicators are in the severe acute malnutrition or moderate acute malnutrition column, that means all the indicators are in the normal range and the child or adult is classified as ‘no acute malnutrition’. You looked at how to measure oedema and MUAC in Study Session 5. Figure 9.1 overleaf reminds you how to do both of these measurements.
What are the criteria used to classify someone as moderately malnourished?
Your answer will depend on whether you are classifying a child or an adult. For example, a child is classified as moderately malnourished if their MUAC is 11-11.99 cm, or if the weight-for-height is in the range of 70-79.99% of the normal range. Children who have oedema are suffering from severe acute malnutrition. For women, having a MUAC of 17-22 cm or a BMI of 16-16.99 indicates moderate malnutrition. However, women with a MUAC between 17-18 cm should be classified as severely malnourished if they have had recent weight loss or chronic illness.
9.2 Principles of management of moderate acute malnutrition
Pregnant women, lactating mothers and children under five are particularly at risk as they have increased nutritional needs. Particular attention is given to these vulnerable groups when trying to address moderate acute malnutrition. The aim of intervention for moderate acute malnutrition (MAM) is to rehabilitate moderately malnourished children, to prevent further deterioration of nutritionally vulnerable groups, and to ensure adequate intake to support pregnancy and lactation.
Local solutions to malnourishment are more likely to have a sustainable impact.
When you are working with families you should always consider what they have available at home and how best the family can support the moderately malnourished woman or child, so that they can become fully rehabilitated. Keep local solutions as the first option as much as possible, since they are more likely to be sustainable. Below are general guidelines to help you manage cases with moderate acute malnutrition.
9.2.1 Where there is no supplementary feeding programme
If the malnourished person is an adult or older child, you can discuss their condition with them. If it is a younger child who is malnourished, then you would talk with their caregiver. Involving the family in discussions helps them to think about why the adult or child may have become malnourished. Your knowledge on causes of malnutrition from Study Session 6 will help you here. You can then provide nutritional advice to the entire family to ensure that the moderately malnourished person takes energy-rich food, as well as more fat and protein in their diet. You can look again at the study session on essential nutrients and food sources if you need to remind yourself about energy-rich foods.
Following up the progress of the moderately malnourished person is very important to encourage continuation of good feeding and caring behaviour (you will learn how to do nutrition counselling in Study Session 11). Plan to do a home visit within one or two weeks of your first visit to see how the family is implementing your recommendations. The aim of your intervention is to move the moderately malnourished person back into the normal range in the table above.
What can you do for a moderately malnourished child where there is no supplementary feeding?
You may have rightly said that you will provide nutritional advice to the family, especially the primary caregiver and follow up the progress by doing a home visit to see if the family is following your recommendations and the child is improving.
9.2.2 Where there is a supplementary feeding programme
Targeted supplementary feeding
There may be a targeted supplementary feeding programme (TSF) in your woreda. You looked briefly at these in Study Session 8. TSF is a programme where regular (three or six monthly) nutritional screening is done in the community followed by provision of blended food either by the health workers or food distribution agents in collaboration with the kebele administration. It is usually organised in a service package of an Enhanced Outreach Strategy and Child Health Days (EOS/CHD). Details of EOS/CHD are discussed later in this study session.
Nutritional advice to families should remain a priority, even in woredas where there is a TSF. However, long-term food security problems may affect the availability of food at home and make it harder for the family to follow your recommendations. Therefore in addition to the nutritional advice you give, targeted supplementary feeding is also usually provided for women and children with moderate acute malnutrition. In addition, people who have been discharged from a therapeutic feeding programme are also eligible for targeted supplementary feeding.
Various cereal-based blended foods are used as supplementary feed in TSF woredas. These cereal blends are composed of precooked cereals and legumes fortified with micronutrients. Commonly used blended foods in Ethiopia are Corn-Soy Blend (CSB), Famix and Unimix. In general, the composition is constituted from 79% of cereals, 20% legumes and 1% vitamins and minerals. In addition to the blended foods, edible oil is given to moderately malnourished women and children.
Supplementary feeding aims to provide the following nutrients:
- 1000-1200 Kcal with 10-15% from protein, 30-35% from fat and 50-60% from carbohydrates.
The recommended monthly ration to ensure the above nutrient intake is:
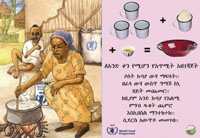
- 6-7.5 kg blended food + 0.9 gm oil + up to 0.6 gm sugar per beneficiary per month. Figure 9.2 shows a poster advertising the rations provided in a supplementary feeding programme.

For practical reasons, 25 kg of blended food is usually given to each beneficiary to use over the next three months together with three litres of oil. Usually, three or six-monthly community screenings are organised in TSF woredas following which the allocation of supplementary food will be made. Children and women with MAM during these screenings are registered and provided with a ration card to ensure they are enrolled into a TSF programme and receive the blended foods and oil. There is no specific discharge criteria in a TSF context; the regular community screenings are used to reassess the nutritional status of children and women, and decide whether they need to continue in (or join) the programme, depending on whether they fulfil the admission criteria.
How many kilos of blended food and litres of oil are given for moderately malnourished child getting TSF ration for three months?
Twenty five kilograms blended food and three litres of oil is provided for each moderately malnourished child as this is considered to provide sufficient nutrients to improve the child’s nutritional status.
Figure 9.3 is a poster showing how rations are used to produce a nutritious supplementary meal.
Supplementary feeding programme
In some woredas, NGOs undertake supplementary feeding programmes (SFPs) to provide support to moderately malnourished individuals. The main difference from the TSF is the opportunity for continuous screening and admission of new cases into supplementary feeding together with continuous follow-up of the weight gain and the condition of the moderately malnourished person. Such a close follow-up also provides an opportunity to assess why a certain child is not progressing as expected and to decide when to discharge those who continue to gain weight.
9.3 Enhanced Outreach Strategy/ Child Health Days (EOS/CHD)
As the name indicates, EOS/CHD is designed to enhance your outreach work as a Health Extension Practitioner to provide certain key activities that contribute to child survival. The Health Extension Programme has activities that should be implemented at household level when doing outreach, and at the health post. For example, an activity you can do during outreach sessions is growth monitoring and promotion; another example would be attending delivery of a labouring woman.
You will be asked to organise CHDs for your kebele. You need to have a good understanding of each aspect of the day, so it will run smoothly. You also need to be able to prepare detailed plans for your kebele. These will be communicated up to the woreda level and will ensure that you receive the required support that you need. While both EOS and CHD signify the same activities, EOS is conventionally used for those woredas where three-monthly enhanced outreach has not yet started. CHD is used to indicate those woredas that have progressed to three-monthly enhanced outreach. It is planned that all woredas will eventually undertake CHD with enhanced outreach every three months. Note that some components will still be undertaken on a six-monthly basis, even in CHD woredas.
9.3.1 Components of EOS/CHD
Activities undertaken as part of EOS/CHD include vitamin A supplementation, deworming, screening for acute malnutrition, social mobilisation for routine immunization and the promotion of infant and young child feeding. The opportunity is sometimes used to provide insecticide-treated nets. Screening for acute malnutrition is done only in food insecure woredas where there is a TSF programme. The overall objective is to enhance child survival by reducing mortality and morbidity in children under five years of age. Your role as a Health Extension Practitioner is therefore critical in supporting this objective.
This section will help you to consider the practical aspects of planning and undertaking EOS/CHD. As EOS/CHD contains many components, you will not be able to deliver the service alone. As a Health Extension Practitioner you will work with additional volunteer community health workers. The number of volunteers depends on the number of services given in EOS/CHD. Table 9.2 below summarises the target group and frequency of EOS/CHD.
| Components of EOS/CHD | Target group | Frequency | |
|---|---|---|---|
| EOS | CHD | ||
Vitamin A supplementation | Children six-59 months | Six-monthly | Six-monthly |
Deworming | Children 24-59 months | Six-monthly | Six-monthly |
Screening for acute malnutrition | Children six-59 months Visibly pregnant women Lactating mothers | Six-monthly | Three-monthly |
Social mobilisation for routine immunization | Age group for routine immunization | Six-monthly | Three-monthly |
Promotion of infant and young child feeding | Families of under-five children | Six-monthly | Three-monthly |
Insecticide-treated nets (ITNs) | Households with under-five child or pregnant woman or lactating mother | Once in three years for long lasting nets | Once in three years for long lasting nets |
9.4 Planning for EOS/CHD
There are two key aspects to planning for EOS/CHD. The first is planning what supplies your woreda will need, the second is mobilising the community so people know about services and support.
9.4.1 Planning for supplies
Before you can plan what supplies you require you need to know the population figures in each of the target groups. This will enable you to estimate the number of tablets or capsules you may need for EOS/CHD. Non-consumable supplies like the MUAC tapes or scissors are needed only if you do not have them in your health post, or the ones you have are damaged. Planning by outreach site may help you to know the number of items you should take with you when conducting EOS/CHD in a particular village. Figure 9.4 shows you the form you should use to help you plans supplies for your village.

What supplies will you need for undertaking EOS/CHD?
The supplies needed include vitamin A capsules, deworming tablets, MUAC tapes, and posters. If ITN distribution is integrated, you will need the ITNs. Albendazole 400 mg, or Mebendazole 500 mg tablets are the most commonly used deworming tablets. You will also need scissors to cut the vitamin A capsules.
You may have also listed weight and height measuring instruments to be used in screening for acute malnutrition. In EOS/CHD these items of equipment are not needed however, because weight-for-height is not one of the measurements used. This is because this measurement takes time to do, and the likelihood of making mistakes in such community screenings is high. There are three instances where there is a risk of making mistakes when measuring weight-for-height; these are when you are taking weight, measuring height and computing the final measurement. Screening for acute malnutrition is done only in food insecure woredas where there is a TSF Programme.
9.4.2 Social mobilisation
Social mobilisation is a critical component of EOS/CHD where the community needs to get clear messages about what are the services; who will receive the services; when the service day for the community will be; where the EOS/CHD will be held for the community being mobilised (see Figure 9.5).

The opportunity is also used to increase the community awareness of the benefits of the components of EOS/CHD and also to increase demand for health services, particularly routine immunization. Community health workers play a critical role in social mobilisation. As a Health Extension Practitioner you may also disseminate the information using the kebele administration and village elders and leaders.
What is the purpose of community mobilisation?
An important purpose is to bring children to a central place so they can receive the services they need. These services will be based on eligibility criteria. It also provides parents and caregivers an opportunity to ask about any concerns they have about their children’s health.
Depending on the size of the kebele, you may subdivide your outreach into a group of villages (outreach site), and decide on a different central location for each of the grouped villages. You should organise yourself to complete the EOS/CHD for all the outreach sites within a short period of time, usually over a maximum of one week.
It is important that the community is informed of the date of the EOS/CHD in advance. Failing to complete an outreach site visit that was in your initial plan could disrupt your next outreach site visit where people will be waiting for you. Therefore, you need to make a realistic plan and stick to this as closely as you can.
9.5 EOS/CHD service organisation
There are a number of aspects you need to consider when planning EOS/CHD service organisation. This section will help you to ensure you make realistic and effective plans.
9.5.1 Outreach site organisation
When selecting an outreach site for EOS/CHD, you should consider the adequacy of the space and suitability of the location for your work in the community. Whenever possible, you should involve the local community leaders in the selection of the site. It should be easily accessible to the community. The outreach site should preferably be in a building or on a veranda or under good shade. It should also have a clear banner/poster indicating that it is outreach site.
Can you give some examples of buildings that could be used as an outreach site?
There will be a number of possible sites in most locations. For example, a school, a kebele administration office, a health post or a church/mosque could be used as outreach sites/posts.
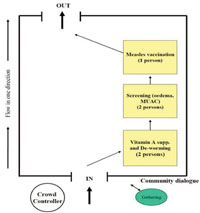
After selecting the site, you need tables and chairs to be arranged in an organised manner so that you can provide the services. You should consider a number of important factors when arranging the flow of the service. First of all you should consider what services are going to be provided in a specific EOS/CHD. As you may recall, some services (such as providing insecticide-treated nets) will not be given in a EOS/CHD. You need to organise the services in a logical order, from a service where a child is least likely to cry, to a service that may create discomfort to a child. For example if there is measles immunization, it should be the last service, as children are likely to cry after the injection and may refuse other services. Figure 9.6 illustrates how the site and flow of services could be organised.
Since mothers may not remember the accurate age of a child in many rural communities, height-age is used as an objective way of excluding children older than 59 months from the service. Height-age is when the age of a child is estimated from its height. A child is expected to be 100 cm tall at the age of five years (60 months). Children taller than 110 cm should not be allowed to receive EOS/CHD services. In some EOS/CHD sites, health workers put up a height age measuring device that looks like a football goal, where the cross-bar is 110 cms high. As you can see in the picture in Figure 9.7, two bamboo sticks are connected with a rope as a cross bar. The rope is measured to be 110 cm from the ground.

9.5.2 Crowd control
The best way to control the crowd is to start the service at the right time. This will help to minimise the length of time mothers and caregivers will have to wait for screening (see Figure 9.8). You should ensure there is enough space between each of the teams providing the different services. As much as possible, arrange the services to facilitate one direction of flow of clients with clear entry and exit points, as you saw in Figure 9.6.

9.6 Registration and referral of cases with acute malnutrition
In Targeted Supplementary Feeding (TSF) woredas where screening for acute malnutrition is integrated with EOS/CHD, the results of your screening are used to identify the people who will get the targeted supplementary foods. Therefore you will be provided with a registration book for you to register all children with malnutrition. Children with either severe acute malnutrition or moderate acute malnutrition are eligible for targeted supplementary feeding and should have their name entered in the registration book.
When you write in the registration book, the information will automatically be carbon copied onto three additional coloured sheets. When you look at a registration book you will see four different coloured sheets. After writing your entries you should send each sheet to different stakeholders, as described below.
- The white coloured sheet remains with the registration book for your records
- The light blue sheet is sent to the woreda food security desk
- The pink sheet is given to the woreda health office
- The yellow sheet is sent to the regional Disaster Risk Management and Food Security Sector (DRMFSS) office.
You should keep the white sheet and submit the other three to your supervisor. He or she will make sure they are sent to the correct recipients. In some woredas, the Food Distribution Agents may take the light blue sheet. Food Distribution Agents are women that are selected from the community to manage the storage and distribution of targeted supplementary foods. They will only give TSF foods for the women and children who are on your list.
You must give a ration card to people with severe acute malnutrition and moderate acute malnutrition. Families will keep these cards to show to the Food Distribution Agent (FDA), so you must make sure that the ration card is not given to someone who is not eligible.
All children and adults with severe acute malnutrition should be treated. If your health post has an Out-patient Therapeutic Programme (OTP) where you can manage cases with severe acute malnutrition, provide the first day treatment and make an appointment for a subsequent follow-up visit.
Study Session 10 looks at how to treat cases with severe acute malnutrition in your health post. For now, you just need to know that if your health post is not yet able to treat cases of severe acute malnutrition, you should refer the child to a nearby health facility where they can access treatment for the appropriate services.
9.7 Reporting
After completing your EOS/CHD activities you have to submit a report. There is a standard reporting template that you will use to fill out the number of children that received each of the components against the target. The performance of your kebele is normally measured by looking at what proportion of the target population that need to receive services have actually received the relevant interventions. You will therefore record information on the reporting template that enables this information to be checked.
In this study session you have learnt about the different anthropometric indices to determine the nutritional status of women and children. You have seen that as a Health Extension Practitioner you have a critical role in helping people in your community who have moderate acute malnutrition. If you apply what you have learned in this and earlier sessions in this Module, you will be able to mobilise and support your community effectively.
Summary of Study Session 9
In Study Session 9 you learned that:
- Anthropometric indices such as mid-upper arm circumference, weight and height are used to determine the nutritional status of women and children.
- The severity of the malnutrition is decided against a set of criteria, including weight for height and body mass index (BMI).
- The presence of oedema always signifies severe acute malnutrition.
- The target group for managing moderate acute malnutrition is children under five, pregnant women and lactating mothers.
- When managing someone who has moderate acute malnutrition, you should identify any problems in the home that led to the malnutrition and then counsel the use of high-energy foods to address the problem.
- Some woredas have Targeted Supplementary Feeding or Supplementary Feeding Programmes which provide additional opportunities for ensuring moderately malnourished people receive energy rich supplementary foods.
- Enhanced Outreach Strategy (EOS) and Community Health Days (CHD) require careful planning to ensure as many adults and children as possible attend and receive services in an ordered and effective way.
- It is important to record accurate information in the registration book, which is then shared with different stakeholders, such as the woreda food security desk and the health office.
Self-Assessment Questions (SAQs) for Study Session 9
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 9.1 (tests Learning Outcomes 9.1 and 9.4)
What are the principles of treatment of moderate acute malnutrition?
Answer
The aim of intervention for moderate acute malnutrition is to rehabilitate children who are moderately malnourished, to prevent further deterioration of vulnerable groups of people (such as pregnant women and lactating mothers) who are moderately malnourished and to support adequate intake of nutritious food for such vulnerable groups. As a Health Extension Practitioner, you need to be aware that children under five, pregnant women and lactating mothers are particularly at risk because they have increased nutritional needs. You will work with families, taking into consideration the kinds of food they have available, to advise them on the most nutritious diet possible. As far as possible, you should explore local solutions to support children and vulnerable women, as this is likely to lead to a more sustainable approach to rehabilitation.
Read Case Study 9.1 and then answer the questions that follow.
Case Study 9.1 Jemila’s story
Jemila Ahmed is a 30 months old girl who came to your EOS/CHD service. Her MUAC was 11.5cm but she did not have oedema. Weight-for-height was not done as it is not part of EOS/CHD
SAQ 9.2 (tests Learning Outcomes 9.2 and 9.3)
- a.How would you classify Jemila’s level of malnutrition?
- b.What actions could you take on the Child Health Day to help improve Jamila’s health?
Answer
- a.Jemila’s MUAC is 11.5cm which comes within the range indicating that she has moderate acute malnutrition (11-11.99cm). As there is no oedema, Jemila does not have severe acute malnutrition, but you would need to monitor her progress carefully.
- b.You could use the opportunity of a CHD to monitor Jemila’s progress and to provide advice to Jemila’s mother or caregiver. Activities undertaken as part of CHDs include vitamin A supplementation and promotion of infant and young child feeding.
SAQ 9.3 (tests Learning Outcome 9.4)
How can a child’s moderate acute malnutrition be managed if there is no supplementary feeding programme in your community?
Answer
If there is no supplementary feeding programme in your community, you can help manage a child’s moderate acute malnutrition in a number of ways. For example you can talk with the primary caregiver why they think the child has become malnourished. You will be able to provide nutritional advice to the whole family to ensure the malnourished child is given more energy-rich food, as well as more fat and protein in their diet.
SAQ 9.4 (tests Learning Outcomes 9.5 and 9.6)
Describe how you would organise services for a Child Health Day (CHD).
Answer
It is important to plan carefully for a CHD and to ensure your community is informed of the date in advance. You need to consider where you will hold the CHD, and that the place you select is in a suitable location with enough space for the services you are going to provide (for example, a school, a health post or a veranda with good shade). An important part of the planning includes organising the services in a logical order, from a service where a child is least likely to cry to one that may create some discomfort to a child. This will also help you to control the direction of the flow of clients through the services. If you start the service at the right time, this will help to minimise the time mother and caregivers will have to wait, and promote effective crowd control.