Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 26 April 2024, 5:11 AM
Nutrition Module: 10. Managing Severe Acute Malnutrition
Study Session 10 Managing Severe Acute Malnutrition
Introduction
In the last session you learnt about the use of anthropometric indices to determine the nutritional status of women and children. You also considered some of the most important methods and principles for managing moderate acute malnutrition (MAM). This session is devoted to giving you a deeper understanding of the way that you can look after children who have developed severe acute malnutrition (SAM). This will start from the steps you need to take to assess for complications and to do the appetite test, so that you are able to identify children who need referral for in-patient management. Then you will learn how to manage the children with severe acute malnutrition who can be cared for in your out-patient therapeutic programme (OTP). Lastly, you will learn how to manage severely malnourished children in OTP using weekly follow-up visits until they reach the discharge criteria.
Learning Outcomes for Study Session 10:
When you have studied this session, you should be able to:
10.1 Define and use correctly all of the key words printed in bold. (SAQ 10.2)
10.2 List the steps for identifying severely malnourished children who require in-patient treatment, and differentiate them from those children who can be treated on an out-patient basis. (SAQs 10.1 and 10.2)
10.3 Describe the admission, referral, and discharge criteria to and from the out-patient therapeutic programme (OTP). (SAQ 10.2)
10.4 Explain the key management and follow-up actions for severe acute malnutrition (SAM) using the OTP protocol. (SAQs 10.3 and 10.4)
10.5 List what information should be entered in the recording and reporting formats. (SAQs 10.3 and 10.4)
10.6 Outline the procedures to organise a health post set up for out-patient treatment of SAM. (SAQ 10.5)
10.1 Severe acute malnutrition: deciding patient management
When thinking about severe acute malnutrition you should have in mind all the vital organs in the body such as the heart, the kidneys and the liver. When a child or adult is severely malnourished, these organs do not function properly. Therefore severely malnourished children are at an increased risk of death if their malnutrition is not identified and treated in a timely way. You need to know the steps required to assess, classify and treat severely malnourished children.
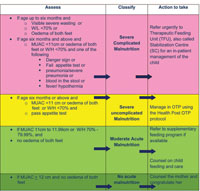
Your first step is to decide whether to provide out-patient management or refer the child to an in-patient facility. Look at the flow chart in Table 10.1 which shows you how to classify the condition of a child and the recommended action you need to take. If you read the table from left to right, you can see how your assessment of the child’s symptoms will enable you to classify the level of malnutrition and whether you need to refer the child to an in-patient facility.
Table 10.1 Flow chart for assessment, classification and action required for malnourished children. (Source: Federal Ministry of Health, 2008, Management of severe acute malnutrition)
Which children with the classification of severe acute malnutrition can be treated at health post level?
As you can see from the flow-chart in Table 10.1, you can treat children with severe uncomplicated malnutrition at health post level, but children with severe complicated malnutrition need to be referred urgently to TFU.
The Federal Ministry of Health has produced guidance (July 2008) on the management of children with severe acute malnutrition at a health post. This provides additional information not covered in this study session.
10.2 Management of severe acute malnutrition
It will not always be easy for you to decide who should be referred to a higher level, or who you should treat yourself at the health post. As you read above this will mainly (but not only) depend on whether the child’s severe acute malnutrition is ‘complicated’ or ‘uncomplicated’. Certain criteria have been established to help you decide whether a child has severe complicated or severe uncomplicated malnutrition:
- Age: all infants under six months of age with SAM need to be treated in an in-patient facility
- The presence of any medical complications, including any of the general danger signs, pneumonia/severe pneumonia, blood in the stool, fever or hypothermia mean that the severely malnourished child is classified as severe complicated malnutrition and must be treated in an in-patient facility. The IMNCI Module looks at each of these complications in more detail. Table 10.2 below gives you a summary of the key complications that you should look for when helping to treat children with severe acute malnutrition.
> means greater than or equal to.
| Complication | Referral to in-patient care when: |
|---|---|
General danger sign | If one of the following is present: vomiting everything, convulsion, lethargy, unconscious, or unable to feed |
Pneumonia | Fast breathing For child six-12 months 50 breaths per minute and above For a child 12 months-five years 40 breaths per minute and above For a child older than five years 30 breaths per minute and above |
Severe pneumonia | A child with fast breathing as indicated above and chest in-drawing |
Dysentery | If blood in the stool |
Fever or Low body temperature | T > 37.5 or febrile to touch T |
Children with poor appetite are also classified as having severe complicated malnutrition and need to be referred to in-patient care. Details on how to test for appetite will be explained briefly below.
10.2.1 The appetite test
![]() A severely malnourished child who has complications should be referred for in-patient care.
A severely malnourished child who has complications should be referred for in-patient care.
Appetite is a very important indicator of the clinical situation of a child who may have malnutrition. A poor appetite means that the child has a serious problem and will need to be referred for inpatient care. Remember that a child who has complications does not need to be given the appetite test and should be referred for in-patient care.
The appetite test: steps to follow
- The appetite test should be conducted in a separate quiet area.
- Explain to the caregiver the purpose of the appetite test and how it will be carried out.
- The caregiver should wash their hands.
- The caregiver should sit comfortably with the child on their lap and should either offer the ready-to-use therapeutic food (RUTF) from the packet or put a small amount on his finger and give it to the child.
- The caregiver should offer the child the RUTF gently, encouraging the child all the time. If the child refuses then the caregiver should continue to quietly encourage the child and take time over the test. The test usually takes a short time but may take up to thirty minutes. The child must not be forced to take the RUTF.
- The child needs to be offered plenty of water to drink from a cup as he is taking the RUTF.
10.2.2 Interpreting the result of the appetite test
Table 10.3 below shows you how to determine whether the child passes or fails the test.
| Minimum amount that a malnourished child should take to pass the appetite test | |||
|---|---|---|---|
| RUTF | BP 100 | ||
| Body weight (kg) | Sachet | Body weight (kg) | Bars |
| ⅛-¼ | ¼-½ | ||
| 4 up to 10 | ¼-½ | 5 up to 10 | ½-¾ |
| 10 up to 15 | ½-¾ | 10 up to 15 | ¾-1 |
| > 15 | ¾-1 | > 15 | 1-1 ½ |
Passes the appetite test
A child that takes at least the amount of RUTF shown in the appetite test table passes the appetite test.
You should explain to the caregiver that the treatment option for the child is OTP. You would then register the child’s OTP card (you will learn how to do this later in this study session).
Fails the appetite test
A child who does not take the amount of RUTF shown in the appetite test table fails the appetite test. You should explain to the caregiver that the choice of treatment for the child is in-patient care; and explain the reasons for recommending this. You would then refer the child to the nearest therapeutic feeding unit / stabilisation centre (TFU/SC) for in-patient management. This is a unit in a health centre or hospital where severely malnourished children with complications or poor appetite are referred and managed. Once the complications improve, these children will be referred back to you for continued out-patient follow-up in your health post.
You may have seen a video on outpatient management of severe acute malnutrition in a training session. If not, when at the health centre try to use the opportunity to see the video if it is available. You will be able to see a child who passes the appetite test and another child who fails the appetite test.
10.3 Management of severe acute malnutrition in OTP
After completing the anthropometry, checking for complications and doing the appetite test, you will know which children with severe complicated malnutrition will be in need of immediate referral and those with severe uncomplicated malnutrition that can be treated at the health post level. As you read earlier, the out-patient treatment programme based on your health post or any other out-patient facility is called an OTP (out-patient therapeutic programme). Once a child is identified as having severe uncomplicated malnutrition, you should explain the condition of the child to the caregiver; register the child in the registration book and also on an individual patient follow-up card called the OTP Card (you will look at how to do this in Section 10.5 below).
10.3.1 Admission procedures
An important part of your role is to explain to the caregiver how to help with the OTP treatment.
You should always make sure that the caregiver is fully aware of the condition of the child, and the need for weekly follow-up visits until the child reaches the discharge criteria. If the condition of the child progresses smoothly, the child normally recovers within five to seven weeks. Some children could take longer, however, and after eight weeks, if there has been nor or little improvement, you will need to stop the OTP treatment and refer the child to TFU. In addition to the need for weekly follow-up visits, you should make sure that the caregiver clearly understands the dosage and frequency of each of the drugs as well as the weekly ration of RUTF to give to the child. It is usually good to ask the caregiver to repeat to you how they will administer the RUTF and drugs after you have finished explaining the details to them. This will enable you to verify if the message has been correctly understood by them.
You also need to register the child and fill out the OTP card (the child’s follow-up card) on the admission day, and continue to use this in the regular follow-up of the child (see Section 10.5 below).
10.3.2 Ready-to-use therapeutic food
Ready-to-use therapeutic food (RUTF) is given during out-patient management of a severely malnourished child. The most commonly known brands of RUTF are Plumpy’nut® and BP-100® (see Figure 10.1). RUTF is ready to use, as its name indicates. That means it does not need cooking, or any other process before feeding the child. It is high energy food contained in a concentrated form, enriched with minerals and vitamins to replenish a severely malnourished child. Table 10.4 below shows you how much RUTF should be given to a child according to their weight in kg.

| Class of weight (kg) | Plumpy’nut® | BP-100® | |||
|---|---|---|---|---|---|
| sachet per day | sachet per week | bars per day | bars per week | ||
| 3.0-3.4 | 1¼ | 9 | 2 | 14 | |
| 3.5-4.9 | 1½ | 11 | 2½ | 18 | |
| 5.0-6.9 | 2 | 14 | 4 | 28 | |
| 7.0-9.9 | 3 | 21 | 5 | 35 | |
| 10.0-14.9 | 4 | 28 | 7 | 49 | |
| 15.0-19.9 | 5 | 35 | 9 | 63 | |
You should explain to the caregiver the following key messages about RUTF so they are able to help with the treatment.
- RUTF is a food and medicine for malnourished children only. It should not be shared
- For breastfed children, always give breastmilk before the RUTF and breastfeed on demand
- RUTF should be given before other foods. Give small regular meals of RUTF and encourage the child to eat often, every three to four hours
- Always offer plenty the child plenty of clean water to drink while eating RUTF
- The caregiver should use soap and water to wash their hands before feeding the child
- Keep food clean and covered
- Sick children get cold quickly, so it is important to keep the child covered and warm at all times.
10.3.3 Routine drugs
In addition to the RUTF, severely malnourished children need to be routinely given drugs using the administration schedule outlined in Table 10.5 overleaf.
| Drug | Treatment |
|---|---|
| Vitamin A | Ask if it has been given in the last six months Give one dose at admission if one not given previously Do not give a dose of vitamin A if the child has oedema |
| Folic acid | One dose at admission |
| Amoxicillin | One dose at admission and give seven days treatment to take home |
| The first dose should be given in the presence of the supervisor | |
| De-worming | One dose in the second week (second visit) |
| Malaria | According to national protocol (see the study session on malaria in the IMNCI module) |
| Measles (from nine months old) | Ask if the child has been vaccinated |
| Give one vaccine on the fourth week (fourth visit) if not given previously | |
| Iron | Not given - iron is already in all RUTF |
As you see from the information in Table 10.5, if a child is admitted to your health post for treatment of severe acute malnutrition you should always give them a dose of vitamin A, unless the child has oedema or has received vitamin A in the previous six months.
![]() A severely malnourished child should be given antibiotics even if there are no signs of infection.
A severely malnourished child should be given antibiotics even if there are no signs of infection.
Note that severely malnourished children should be given antibiotics (Amoxicillin) even if they do not have signs of infection such as fever. Fever results from an immune response of the body to an infectious agent. As a severely malnourished child has a very weak immune system, it often fails to develop a fever response. Therefore a severely malnourished child should be given antibiotics without waiting for typical signs of infection.
Always make sure that the caregiver gives the child the first dose of the drugs in your presence. This will give you an opportunity to make sure that they are able to administer it appropriately. The caregiver can then confidently replicate what they have done in your presence, when caring for the child at home.
After completing the anthropometry and deciding whether a child is severely malnourished, what must you do next to decide whether a child needs to be treated as an in-patient?
You should first consider the child’s age because children under six months with SAM always need to be cared for in an in-patient faculty. You would then check for the presence of complications and finally you would do the appetite test.
10.4 Follow-up of severely malnourished children in an OTP
There are a number of steps you need to take when following up the treatment and care of severely malnourished children in an OTP. These are outlined below.
10.4.1 Weekly follow-up
The information mentioned in these steps is also indicated on the OTP card which will help you to remember all the essential points to check.
Step 1: Ask about
- Diarrhoea, vomiting, fever or any other new complaint or problem the child may have
- Whether the child is finishing the weekly ration of RUTF.
Step 2: Assess for
- Complications
- Temperature, respiration rate
- Weight, MUAC and oedema.
You should then do the appetite test.
Step 3: Decide on what action to take based on the above follow-up assessment
Refer if there is any one of the following:
- Development of any complications
- The child fails the appetite test
- There is an increase in the level of oedema. For example, if the oedema was only on the feet during admission, and the child has developed increased swelling on higher parts of the body such as the legs or the face
- A child who did not have oedema on the preceding visit is now presenting with oedema on the current visit
- A child without oedema loses weight for two consecutive visits. A child with oedema has abnormal fluid accumulated in the body. As a result, when the condition starts to resolve with the treatment you are administering, and the oedema fluid starts to be lost from the body, you might expect to see a decrease in body weight
- A child with oedema, or one who has recovered from oedema, fails to gain weight for three consecutive visits
- Major illness or the death of the main caregiver so that the child can’t be managed at home.
If there is no indication for referral, provide the weekly follow-up OTP services. These include:
- Providing any routine drug that needs to be given on the current visit according to the guidance in Table 10.5
- Providing the weekly ration of Plumpy’nut®
- Making an appointment for next weekly follow-up
- Recording the relevant information on the OTP card.
If the child is absent for any follow-up visit:
- Ask a Community Volunteer to do a home visit and report back to you
- If there is another child with severe uncomplicated malnutrition in your follow-up from the same neighborhood, you may also ask the caregivers why their neighbour didn’t come to OTP follow-up.
10.4.2 Home visits
You may face a difficult situation where the family of a child who needs referral refuses to take the child to an in-patient facility. Or sometimes you may not be sure about the presence of a particular complication and whether to refer a child or not. In such instances, you need to organise a home visit in between the OTP days to follow the progress of the child. If a child is not gaining weight while taking the Plumpy’nut®, you may also want to do a home visit to understand if there is inappropriate sharing of food at home which means the child is not receiving enough nutritious meals.
In all instances of home visits, try to assess the child in exactly the same way that you would assess them during a routine weekly follow-up in your health post. In addition, do your best to provide psychological support to the family in order to encourage them to care for the child properly. Discuss with the family if there are any factors that are preventing them from following your earlier advice.
10.4.3 Discharge
You should discharge the child from OTP follow-up if the following criteria are fulfilled:
- For those who were admitted based on oedema: discharge if there is no oedema for two consecutive visits (14 days)
- For those who were admitted without oedema: discharge when the child reaches discharge target weight.
If the child fails to reach the discharge criteria after two months of OTP treatment, you should refer the child for in-patient care and undertake more detailed follow-up to investigate the cause.
On discharge make sure:
- Counselling is given to the mother or caregiver about child feeding and care
- Wherever the service exists, give a discharge certificate to the caregiver and make a referral to the supplementary feeding programme
- Each child is registered appropriately in the registration book on date of discharge.
10.5 Recording and reporting
Keeping accurate records for each patient with OTP who visits your health post and for each home visit you make is a key part of your job. There are a number of different forms for recording information and in this section you are going to learn about these and why it is important to keep good records.
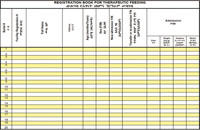
10.5.1 The registration book
The registration book is used to keep a record of children with severe uncomplicated malnutrition who are admitted to the OTP in your health post. The registration book is filled in only on date of admission and date of discharge. The information in the registration book will enable you to prepare monthly reports and analyse the performance of your OTP. The registration book is arranged in such a way that the admission information is written on the left-hand side page of the book while discharge information for the same child is completed on the next sheet on the right-hand side. You can see this in Figures 10.2 and 10.3, which reproduce sections from the registration book. Alternate rows are coloured to ease completion of information both on the date of admission and on the date of discharge.
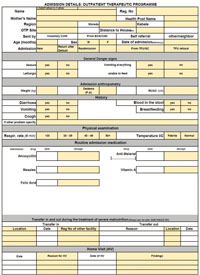
10.5.2 The OTP card
The OTP card is a patient follow-up card that is used to help in your management of severe uncomplicated malnutrition. This card basically provides you with an opportunity to record information about children efficiently on a weekly basis. There is space for each key indicator to be filled out in an organised manner. Most of the front page of the OTP card is filled in on the date of admission. It provides relatively detailed information on the child’s identity, clinical history, physical examination, the anthropometric indicators warranting admission and also the medication given on the date of admission. You can see a copy of this part of the OTP card in Figure 10.4.
You can also see that low down on the front page there is space to write whether the child is transferred or not, and another space to write your findings in case you decide to do a home visit.
The back of an OTP card is dedicated to the weekly follow-up visits of children with severe uncomplicated malnutrition. There are twelve columns, representing one week each (see Figure 10.5).
Why won’t you be expected to manage children who are less than six months of age at your health post?
As you may remember, all children under six months old classified as having severe acute malnutrition have to be referred for in-patient care.
What is the maximum stay on OTP if a child does not reach the discharge criteria?
It is eight weeks, because if the child fails to reach the discharge criteria after this time they should be referred for in-patient care and detailed follow-up.
10.5.3 Monthly reporting
When reporting on children with severe uncomplicated malnutrition, you need to follow a standard format. Information provided by you will include data on new admissions, transfer to in-patient facilities, children cured, children defaulting from treatment and the number of children who have died. The OPT card data is recorded according to the child’s age group and enables a picture to be built up in relation to the outcomes for children in the programme. It is therefore important that you keep accurate and clear records.
What admission procedures should you undertake once you classify a child as having severe uncomplicated malnutrition?
You would be able to manage this child at your health post. You would need to explain the procedures of OTP treatment to the child’s caregiver, register the child in the registration book and issue an OTP card for detailed follow-up visits.
10.6 Organisation of the health post to manage cases in OTP
You need to be organised so you can manage children with severe uncomplicated malnutrition effectively in your health post. Being organised will help you to anticipate the items you need, and arrange the timing of visits so that your work is efficient and the children you manage receive optimum care.
10.6.1 Supplies
Table 10.6 overleaf sets out the items you need to treat children with severe acute malnutrition in your health post. The minimum stock indicated has been calculated by assuming you have a caseload of 30 severely malnourished children in your health post. Experience shows that the caseload varies significantly from woreda to woreda; however, your health post may have a much lighter caseload. Based on the caseload in your health post, you should talk with your supervisor and woreda health office to ensure availability of the items set out below.
| Item | Minimum stock/month |
|---|---|
| Ready to use therapeutic foods | 4 cartons/week or 16 cartons/month |
| Amoxicillin | ½ tin |
| Mebendazole 100 mg | 1 tin of 100 tablets |
| Folic Acid | 15 tabs |
| Vitamin A capsule | 30 capsules |
Measles vaccine vials (10 doses) | (Number of targeted children x measles coverage/10) +10% |
| Plastic cups | 2 |
| Drinking water | 1 Jerry can |
| Salter scale (25 kg) plus pants or plastic basin | 1 |
| MUAC tape | 2 |
| Thermometer | 1 |
| Soap for hand washing | 1 |
| OTP card | 30 |
| Registration book | 1 |
| Stock card/supply register | 1 |
10.6.2 Community mobilisation
Community mobilisation is a process of capacity building in which individuals, groups and communities carry out activities on a voluntary, fully participatory basis for a commonly agreed goal. The goal of community mobilisation in the context of the management of severe acute malnutrition is to raise awareness of what malnutrition is and where and how to seek treatment using the OTP services available at the health post. Raising awareness, early case detection, giving information on appropriate childcare, reduction of defaulting and creation of a sense of ownership by the community are among the aims of community mobilisation.
To instigate community mobilisation effectively you need to map what formal and informal communication structures exists in the community. You need to identify respected men and women in the community that people would listen to. If you convince them of the need for managing severe acute malnutrition, then it will be a lot easier for you to convince other residents in the same community. You can even ask the respected elders to talk to their villagers. For example, you could use the formal communication channels — including the kebele administration and Gott leaders — and ask them to use one of their meetings to pass on key messages.
The content of the key messages may be different depending on your aims, for example, whether you want to emphasise the importance of follow-up of children on treatment, or raise community awareness on the subject of acute malnutrition. Community mobilisation is looked at in more detail in the Health Education Module.
10.6.3 Assignment of OTP days
All OTP cases of severe uncomplicated malnutrition need to have a weekly follow-up at the health post. It is usually advisable to fix one day every week for the OTP activity, including follow-up. For example, you may choose every Tuesday to be an OTP day. This will enable caregivers to remember the day of their appointment. If they miss one of the appointments, they can then come on the subsequent Tuesday. If you identify a severely malnourished child on another day of the week, you may decide to give a ration adequate until the usual OTP day, or you may decide to give RUTF ration to cover until the next OTP day in the subsequent week so that the child is not brought back to the health post twice in a a few days. For example, if you identify a severely malnourished child on a Friday while your usual OTP day is on Tuesday, you may decide to give RUTF ration for ten days so that the child comes on the Tuesday that falls ten days later. After that, you can continue the weekly follow-up for the child on every Tuesday. Remember to consider important events in the community that may affect attendance when choosing the most effective OTP day, such as market day or a religious worship day.
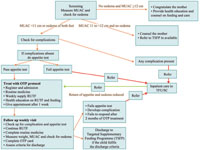
This study session looked at the important steps you should take when managing a child with severe acute malnutrition. The flow chart in Figure 10.6 summarises these steps.
You can see from the flow chart the key steps that are necessary when managing severe uncomplicated malnutrition of a child during the different phases of treatment. The red arrows indicate referrals, while the green arrows indicate the children you had referred who have come back to you once their complication improves. The black arrows indicate the flow of treatment as the child progresses over the course of treatment.
Summary of Study Session 10
In Study Session 10 you learned that:
- All infants under six months with SAM need to be treated in an in-patient facility.
- The presence of medical complications, including general danger signs, or failing the appetite test means that a severely malnourished child should be classified as severe complicated malnutrition and referred to an in-patient facility.
- Children of six months or older with severe uncomplicated malnutrition can be treated in an OTP at your health post.
- There are admission, referral and discharge criteria to and from OTP.
- The OTP protocol provides you with the key steps for managing children with severe acute malnutrition.
- It is important to record information on the appropriate registration and recording forms.
- There are different aspects for organising out-patient treatment of SAM, including community mobilisation and using formal communication channels to ensure your community are aware of the relevant services.
Self-Assessment Questions (SAQs) for Study Session 10
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
Read Case Study 10.1 and answer the questions that follow.
Case Study 10.1 Dawit’s story
Dawit Alemu is a 36 months old boy who is brought to your health post with the complaint of swelling of both of his feet. When you press his feet, the skin does not return to normal for two seconds. You measure Dawit’s MUAC (11.5cm), his weight (9 kg) and his height (86.5cm).
SAQ 10.1 (tests Learning Outcome 10.2 )
- a.How would you classify Dawit and why?
- b.What additional information do you need to be able to decide whether to refer Dawit to the health centre or hospital?
Answer
- a.Dawit’s MUAC is in the ‘moderate acute malnutrition’ range because his MUAC is between 11cm and 12cm. Look back at Table 5.3 if you need to remind yourself of the different ranges of MUAC. His weight for height is also in the ‘moderate acute malnutrition’ range because it is between 70% and 80% of what would be the normal weight for an infant of his age. However you would class Dawit as having ‘severe acute malnutrition’ because he has oedema. Any child who fulfils one criterion for severe acute malnutrition (and oedema falls into this category) will be classified as having severe acute malnutrition.
- b.Because Dawit is six months old, he does not automatically need to be referred to an in-patient facility. If Dawit had complications however – such as the presence of general danger signs, pneumonia/severe pneumonia, blood in the stool, fever or hypothermia – his classification will be ‘severe complicated malnutrition’. This means he needs to be referred to an in-patient facility for stabilisation of his clinical condition. Another indicator that would require Dawit to be referred to an in-patient facility would be if he failed the appetite test. You should recall that in the appetite test, there is a minimum amount of food that the child should take for their weight range. For Dawit, because his weight comes in the range of 4 – 10kg, he needs to take ¼ – ½ of a sachet to pass the appetite test. If he does not pass, then he needs to be referred.
SAQ 10.2 (tests Learning Outcomes 10.1, 10.2 and 10.3)
- a.Explain the importance of the appetite test.
- b.When would you admit a child to an OTP and what procedures should you follow?
- c.What advice would you give to a mother or caregiver whose child is taking Plumpy’nut®?
Answer
- a.The appetite test is an important indicator of how seriously malnourished a child may be and whether they need to be referred for in-patient care. A child who is unable to take the minimum amount of RUTF required to pass the appetite test should be referred to and receive care from the nearest Therapeutic Feeding Unit or Stabilisation Centre for in-patient management.
- b.If a malnourished child does not need referring to an in-patient facility they can be registered for an Out-patient Therapeutic Programme (OTP). You should explain to Dawit’s family how to help with the OTP treatment and then you would register Dawit in the OTP registration book, and fill out the OTP card which will allow you to build up a record of his treatments and progress.
- c.There are a number of key messages that you can give the parents — compare your answer with the messages in the list below. You may want to write these in your Study Diary to refer to when following up children on an OTP day, as a reminder of the points you want to share with parents.
- Plumpy’nut® (RUTF) is a food and medicine for malnourished children only. It should not be shared
- For breastfed children, the mother should always give breastmilk before the RUTF; she should continue to breastfeed on demand
- RUTF should be given before other foods. The mother or caregiver should give small regular meals of RUTF and encourage the child to eat, every three to four hours
- The child should always be offered plenty of clean water to drink while eating the RUTF
- The mother or caregiver should always use soap and water to wash their hands before feeding the child
- Food should be kept clean and covered
- Sick children get cold quickly, so the child should be kept covered and warm.
SAQ 10.3 (tests Learning Outcomes 10.4 and 10.5)
- a.Explain the importance of the registration book and OTP card for the management of children in your community who have severe uncomplicated malnutrition.
- b.What indicators will you look for at follow up visits to a child with severe uncomplicated malnutrition who is being cared for at home?
Answer
a.The registration book is used to enable you to prepare monthly reports and analyse the performance of your OTP. You will be able to compare the monthly performance of your health post with other health posts and with the standard that is set at your woreda or regional level. You can also see the trend of mortality rate and/or recovery rate over several months to see if your efforts to improve the quality of the OTP services are bearing fruit.
The OTP card enables you to follow children efficiently on a weekly basis. You have to record each key indicator for the child and this will help you follow up the child’s progress in the course of the treatment (and remind you which ones you need to check). You should explain to the parents or caregiver the importance of the registration book and OTP card for the management of children in your community who have severe uncomplicated malnutrition, so they know why you are taking this information.
- b.When you make follow-up visits to the home, you will want to see how the malnourished child is progressing. You would ask the parents or caregiver whether the child has had diarrhoea, vomiting, fever or any other new complaint or problem since the last visit. You would also want to ensure that the child is finishing the weekly ration of RUTF. Other indicators you need to look for include whether there are any other complications, the child’s temperature, weight and MUAC. You should also check whether the child has oedema and finally, do the appetite test.
SAQ 10.4 (tests Learning Outcomes 10.4 and 10.5 )
When can a child with severe acute malnutrition be discharged from an in-patient facility and what advice would you give the parents or caregiver?
Answer
If a child was admitted to an in-patient facility with oedema on both feet, there needs to be two consecutive visits (14 days) where there is no presence of oedema before the child can be discharged. For a child who was admitted without oedema, the criterion for discharge is when the child reaches its target weight. On discharge from the facility you would need to counsel the mother on feeding and caring for her child at home. If the service exists, you can provide the mother or caregiver with a discharge certificate and make a referral for the child to the supplementary feeding programme.
SAQ 10.5 (tests Learning Outcome 10.6)
What steps will you take to ensure that the OTPs you organise are well attended and run effectively?
Answer
There are different ways to ensure that your community is aware of the services available in OTPs. Using formal and informal ways to communicate with people (e.g. talking to respected men and women in your village who other people will listen to, so they can promote awareness of OTP days) will be important. You can also ask kebele administrators and Gott leaders to use their meetings to pass on key messages. Assigning a fixed day in the week as an OTP day will help caregivers to remember the day of their appointment. If you plan ahead and anticipate the stocks you need, based on your caseload, this will help ensure you can provide the best possible treatment and care for managing severe malnutrition in your community.