Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 22 January 2026, 1:40 AM
Postnatal Care Module: 4. Preparation for Postnatal Care
Study Session 4 Preparation for Postnatal Care
Introduction
You are aware of these considerations from the Modules on Antenatal Care and Labour and Delivery Care.
In the majority of pregnancies prior to delivery, you will have already started communicating and discussing postnatal care with the mother and other family members. It is during these antenatal visits that you will be able to collect information about the mother, the family and their social conditions, and you will also be able to give them your address and tell them how they can contact you whenever they need your assistance. During the pregnancy you will also have encouraged all mothers to deliver their baby in the Health Post or higher health facility if possible, but in rural Ethiopia over 94% of women will deliver at home. In those cases, you will have advised the family members to call you immediately when labour starts.

If you are present at the delivery, you already know that you should stay with the mother for at least the first six hours after the birth. However if she gave birth without you, visit her as soon as possible, ideally within a few hours and no later than the first day. Before you go to the mother for the first postnatal visit, prepare the equipment and drugs that are essential to provide effective postnatal care. In this study session, you will learn about the equipment, the schedule and aims of the postnatal visits, the detailed steps of necessary preparation before you go, and what you should do when you reach the new mother’s home.
Learning Outcomes for Study Session 4
When you have studied this session, you should be able to:
4.1 Define and use correctly all of the key words printed in bold. (SAQ 4.1)
4.2 Explain why the home visit is a critical opportunity to provide postnatal care and describe the current barriers to universal facility-based postnatal care in Ethiopia. (SAQ 4.2)
4.3 Describe the recommended schedule for postnatal home visits in uncomplicated cases and in cases that need specialised care. (SAQ 4.1)
4.4 Describe the preparations, equipment and drugs you should take before you leave for a postnatal home visit. (SAQ 4.3)
4.5 Describe the key steps to follow while conducting a postnatal home visit, including ways to increase confidence among family members in your professionalism and ability. (SAQ 4.3)
4.6 Explain the importance of using effective counselling skills to deliver health messages on postnatal care and know how to check that mothers have understood. (SAQ 4.3)
4.1 Home visits: the best opportunity to provide postnatal care
The ideal way to provide maternal and child health services is through health care delivered by skilled personnel in a health facility. However in Ethiopia there are many challenges to achieving this goal, such as shortage of trained health workers and facilities, and difficulties of access for rural populations to facility-based health care – including postnatal care.
It may take many years to solve all these challenges. Therefore, while working hard to strengthen the health system and improve access to facility-based care in rural communities, your current role as a Health Extension Practitioner is to focus on home visits for the delivery of postnatal care.
4.1.1 Barriers to facility-based postnatal care
Before you introduce a postnatal care (PNC) service in your community, you should first know about the barriers and fully understand why home visits remain the optimum PNC service delivery method in rural communities. The most important barriers hindering facility-based postnatal care are:

- Social and cultural barriers: The tradition of keeping mothers and newborn babies indoors for a few days after the birth in a period of seclusion, and certain community rituals during this period, hinders mothers from going to health facilities for PNC. You should gradually explore these barriers in your locality and work together with the community leaders to change these practices.
- Geographic barriers: Walking across mountains, crossing rivers without bridges during the rainy season, and lack of roads, are some of the geographical barriers that hinder mothers from accessing health facilities for PNC (Figure 4.1).
- Physical access: Even though some mothers would prefer to go to a health facility, the nearest health centre or hospital is not within a reachable distance on foot or with available transport.
- Financial barriers: In Ethiopia, health services for labour and delivery and postnatal health services are considered to be free of charge, but in reality families have to pay for transport for the woman to the health facility, and for consumables including drugs and surgical gloves. These extra costs remain a major barrier to facility-based care.
- Quality barriers: After reaching the health facility, the mother and newborn may not get the expected quality of PNC service because of lack of adequately trained health workers, or shortages of equipment or drugs. Poor quality services reduce confidence in other mothers in the community, who are less likely to make the effort of going to the health facility.
An important secondary target for your PNC visits is to explore some of the social and cultural barriers mentioned above and work with community leaders to try to change these. Study Session 1 of this Module described a number of ways in which you might do this. Thinking back to that, now write a short action list of things you would try to do.
There are many things you might have included. Go back to Study Session 1, Section 1.6, and compare your answers with the ideas put forward there.
4.1.2 Evidence that home visits improve the effectiveness of PNC
Unfortunately, there is not much evidence from research on home PNC visits in Ethiopia to serve as a model of best practice that can be replicated in every region of the country. However, there are experiences and evidence from South Asia that show significant results in improving PNC coverage and reducing the maternal and neonatal mortality rate within a short period of time, using a home-based approach. Of course, there will be cultural differences between countries, but the results are encouraging. For example, studies conducted in India, Bangladesh and Pakistan have shown that home visits can reduce deaths of newborns by 30-61% in developing countries where there is high mortality. In particular, home visits improved coverage of the key high-impact and cost-effective neonatal interventions such as:
- Early initiation of breastfeeding
- Skin-to-skin contact between newborns and their mothers (Figure 4.2).
- Delayed bathing of the newborn until at least 24 hours after the birth
- Attention to hygiene, such as hand washing with soap and water
- Hygienic care of the baby’s umbilical cord stump.

We will refer to each of these interventions later in this study session, or later in this Module. For now, you should simply note that although we do not have comparable Ethiopian research, these South Asian findings provide sufficient evidence of the key elements needed for effective home-based postnatal care in Ethiopia.
4.2 Schedule for postnatal home visits
Currently, there is enough evidence and full consensus on key elements of essential postnatal care to improve the health and survival of newborns and mothers. However, it is still difficult to find evidence-based recommendations that can be taken as a standard for the optimal timing and frequency of postnatal care contacts. Different South Asian countries have evaluated different timings, but almost all of them have visited mothers at least two to three times in the first week after the birth. In all cases the first visit was within 24 hours after the delivery of the baby.
As you already know from Study Session 1 of this Module, the first 24 hours and the first seven days are the crucial times when most mothers and newborns die. Based on the available information from the experiences of other countries, and the feasibility of applying each option in Ethiopia, the World Health Organization has recommended a schedule of visits for postnatal care. For all normal deliveries with an outcome of a full term and normal birth weight baby, the recommended frequency of home visits should be as follows:
- The first visit should take place within 24 hours of the birth; whenever feasible do the visit as early as possible.
- The second visit is on the third day after the birth.
- The third visit is on the seventh day after the birth.
- The fourth visit is during the sixth week after the birth.
The Module on Integrated Management of Newborn and Childhood Illness will teach you specific details of these additional postnatal visits.
Additional visits are needed on the fifth and tenth day after the birth in special circumstances, for example in:
- preterm babies, i.e. those delivered before 37 weeks of gestation
- low birth weight babies, i.e. those weighing less than 2.5 kg
- all sick mothers and newborn babies
- HIV-positive mothers.
Family members should also send for you to come immediately if a mother or the baby has a problem at any time during the postnatal period. Some families may be reluctant to bother you, so it is important that you always reassure each family that contacting you is the right thing to do if they become worried about the health of the mother or the baby.
4.3 Preparations for a postnatal home visit
4.3.1 Personal hygiene

Before you attend for a home visit, make sure you have taken care of your own personal hygiene with particular emphasis to your hair, nails and clothes. This instruction may seem very basic and simple, but a poor appearance and lack of hygiene can have a negative effect on your relationship with the community and families and can also easily affect the credibility of your work. Always wear simple but very clean clothes when you go for a home visit to provide PNC (Figure 4.3).
Why else is it important to emphasise hygiene? Think back to what you learned in some of the earlier study sessions in this Module.
Scrupulous attention to cleanliness and hygiene during birth and postnatal visits helps to prevent postpartum infections. If you stress your own personal hygiene it will be easier to persuade the mother and her family of the importance of cleanliness if her next baby is a home birth.
4.3.2 Equipment
Put the items listed in Box 4.1 into your bag, which should be specially prepared to carry supplies during home visits.
Box 4.1 Equipment for a postnatal home visit
- Salter scale to weigh the baby
- Blood pressure measuring apparatus
- Stethoscope

- Thermometer
- Wrist watch or timer, to help you count the mother’s pulse and the baby’s respiration rate

- Soap for washing your hands
- A clean towel to dry your hands
- Vitamin A capsules
- Iron and folate tablets
- Tetracycline eye ointment
- Counselling card and screening card for PNC.
- Record book, referral form and pen.
You will be given the counselling and screening cards and referral forms for your area. There may be variations in the exact wording and appearance in different regions, but they all cover essentially the same points.
4.4 Key steps to follow while conducting a home visit
To creating a caring environment and to develop confidence in your ability among the family members, you should apply the following practices:
- Know and show that you respect the local beliefs, culture and norms during communication.
- Greet everyone using the local terms.
- Explain the reasons for the visit to the mother and family members, using simple words in local language.
- Allow enough time for general conversation and confidence building.
- Act with confidence, and speak confidently with a gentle tone and voice.
- Be respectful to every member of the family.
Ask about the well being of the mother and the baby and discover whether either of them have any health problems, or if there is any difficulty in making the adjustments to having a new baby in the family. Use the standard screening approach: ask, check, classify and take action. The most critical task is to use the screening cards to help you to identify any life-threatening conditions or general danger signs in postpartum mothers and newborns. You already learned how to do this in Study Sessions 1 and 3.
Using the counselling cards, counsel the mother about her own health and the baby’s health and condition. Always check her understanding after counselling (see Section 4.5 below).
Complete the postnatal home visit form and make an appointment for the next visit. Thank everyone for making you welcome in their home.
4.5 Counselling mothers during the postnatal period
To standardise the counselling of mothers during home visits for PNC, you should use the counselling cards issued by your Regional Health Bureau. When counselling mothers, it is always important to use the following skills:
- Ask and listen: Find out what the mother is already doing for her child and herself by asking thoughtful questions and listening carefully to her answers. Then you will know what she is doing well, and what practices need to be changed.
- Praise: Praise the mother for something helpful she has done. It is likely that she is doing something helpful for herself and the newborn; for example, she may be eating a good diet, breastfeeding the baby exclusively, and keeping herself and her baby clean. Be sure that the praise is genuine, and only praise actions that are indeed good for her health and that of her baby.
- Advise: Limit your advice to what is relevant to the mother at this particular time. Too much advice, or advice given at the wrong time, can be overwhelming and the mother may ignore it. Use language that the mother will understand. If possible, use pictures, screening cards, or real objects to help explain clearly what you want her to do, know or understand.
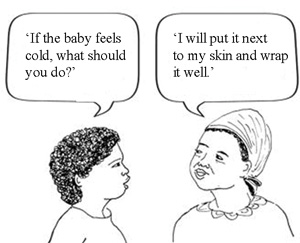 Figure 4.4 Check carefully that the mother has understood your health messages.
Figure 4.4 Check carefully that the mother has understood your health messages. - Check understanding: When you explain something to the mother, ask questions to find out what she understands and what needs further explanation (Figure 4.4). Avoid asking leading questions (that is, questions which suggest the right answer to her even if she does not understand); also avoid questions that can be answered with a simple yes or no, because they do not help you to check exactly what the mother has understood.
The critical maternal health issues that you should address during counselling in postnatal home visits are shown in Box 4.2.
Box 4.2 Health issues to counsel the mother on
- Identification of general danger signs
- Emotional support
- Support for maternal nutrition
- Establishing optimum breastfeeding
- Hygiene and infection prevention
- Support for family planning
- Special care for HIV-infected mothers
- Early care seeking for the mother and the newborn baby if problems arise
- Routine care of a normal baby.
You will learn about these issues in more detail in later study sessions in this Module.
You are on your second visit to a mother of a newborn baby delivered at home. She tells you the baby is crying a lot, that she has had little sleep, and is feeling sore and very run down. What do you do?
Obviously you need to find out more. Is the mother finding it difficult to feed the baby – might she have mastitis? Have mother or baby got an underlying infection, e.g. problems with the umbilical cord stump in the baby, or a perineum wound infection in the mother? Is she getting the extra nutrition she needs, and are her family and community supportive? If your initial questioning (and examination if necessary) satisfies you that there is nothing seriously wrong, then you can advise her accordingly. If you think there may be something more serious, you should consider referral.
Summary of Study Session 4
- The major barriers to facility-based PNC are social and cultural, physical, geographic, quality and financial barriers. The home visit-based approach is the one that addresses all these barriers most effectively in rural communities.
- The schedule of PNC home visits for uncomplicated mothers and newborns is: first visit within 24 hours of the birth, and visit again on day three and day seven, and during the sixth week.
- For all sick mothers and newborns, HIV-positive mothers, preterm and low birth weight babies, you should also visit on day five and day ten.
- When you conduct a home visit for PNC, always wear simple but very clean clothes, and pay attention to your personal hygiene.
- Don’t forget to pack the essential equipment and drugs necessary to provide PNC.
- Be respectful to everyone in the home when you visit; act confidently and communicate clearly using local language and terminologies.
- Use the cards and forms provided to ensure that you cover all aspects of screening and counselling, especially detecting danger signs in the mother and newborn.
- When you counsel mothers, you should ask and listen, praise positive behaviours, limit advice to what she needs to know at each visit, and check that she has understood your messages.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 4.1 (tests Learning Outcomes 4.1 and 4.3)
You are planning the postnatal care of a mother with a preterm baby who is also a low birth weight baby. Define these classifications. Then set out your planned schedule of care indicating how (and why) it differs from the schedule of care that you would plan for a normal weight, full term baby.
Answer
A preterm baby is one delivered before 37 weeks of gestation. A low birth weight baby is defined as one weighing less than 2,500 gm. Ideally, given that this baby is preterm, you would hope that the family would have alerted you in time to be present at the birth. If not then you need to get there as quickly as possible within the first 24 hours. After that: you will need to plan your visits for the third, fifth, seventh and tenth days after the birth and then during the sixth week after birth. The visits on the fifth and tenth days are additional to the kind of schedule you would have for a normal delivery, and this reflects the greater risks of the early neonatal period (the first seven days) if the baby is premature or low weight.
SAQ 4.2 (tests Learning Outcome 4.2)
In an ideal world, all Ethiopian mothers would go to a high quality health facility for their postnatal care. What are the main reasons why this is not currently feasible and why is the home visit therefore so important?
Answer
The main barriers to facility-based postnatal care are set out in Section 4.1.1. Check your answers with the points made there. Did you think of any other barriers, perhaps from your own experience? If so, that’s good.
Home visits are so critical in the postnatal period because of the huge difference that home visits can make to the overall survival rates of newborns. Studies of the South Asian experience have indicated reductions in mortality of between 30% and 61% through home visits. The kind of interventions are set out in Section 4.1.2.
SAQ 4.3 (tests Learning Outcomes 4.4, 4.5 and 4.6)
You are planning a visit to Abrihet. She is a young mother who had her first baby 10 days ago. You have visited her before, but she is very shy and it is taking you time to get to know her and her family. You are getting ready to leave and wondering how you can gain everybody’s confidence.
- a.While packing your bag, you think about checking whether you have everything you need for a postnatal visit and you write a quick reminder to yourself for next time. What did you write?
- b.Then you also write down a few further thoughts about things to remember when you meet Abrihet next time. What did you write?
Answer
Here are some things you might have written down:
Equipment bag
Things I must remember to check have not run out – Vitamin A capsules, iron tablets, tetracycline ointment etc. and soap!
Clean towel? Wrist watch? Enough counselling and screening cards? Record book, pen and referral forms?
All the usual equipment that stay in the bag: scales, stethoscope, blood pressure apparatus, thermometer, etc.
And I had better remember to check if I look clean and neat myself!
But how am I going to get Abrihet to feel more comfortable? These are just a few of the questions I might ask myself:
‘Perhaps I am not using enough local terms, so maybe her family thinks I don’t respect their customs. I wonder if I sound too bold and pushy – must remember to be gentle and to give plenty of time for more general conversation so she begins to relax. It’s so difficult as there is so much to do, that I am often in too much of a rush. I know she listens to me but perhaps I am overwhelming her with too much advice. I’ll try a bit more praise and do more listening myself this time and maybe that will help’.