Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 8 March 2026, 5:10 AM
Postnatal Care Module: 6. Routine Screening of Newborns for Life-Threatening Conditions
Study Session 6 Routine Screening of Newborns for Life-Threatening Conditions
Introduction
In this study session, we return to the general danger signs that the newborn may be at risk, which were already outlined briefly in Study Session 1. This time we focus on assessment and classification of the danger signs in much more detail, and describe the actions that you need to take to prevent and treat common neonatal problems, particularly infections of the respiratory system, eyes and cord stump, and life-threatening conditions such as jaundice and tetanus. Involving the mother in this process is a key part of postnatal care. Her vigilance and willingness to contact you if she is concerned about her baby’s condition can save her baby’s life.
Learning Outcomes for Study Session 6
When you have studied this session, you should be able to:
6.1 Define and use correctly all of the key words printed in bold. (SAQs 6.1, 6.2 and 6.3)
6.2 State the important questions that you need to ask the mother in order to check her newborn baby’s condition. (SAQ 6.3)
6.3 Identify the general danger signs in the newborn and describe the actions to be taken. (SAQ 6.2)
6.4 Describe how to prevent or reduce the risk of infection in newborns. (SAQ 6.3)
6.1 Your first actions before assessing a newborn
Before you start assessing a newborn baby, take off any rings, bracelets or other jewellery, and wash your hands thoroughly with clean water and soap for at least two minutes. This is one of the most important infection prevention actions you can do. Make sure you take your own soap and a clean towel to every postnatal visit, and follow the instructions in Figure 6.1.
You should also show the mother how to wash her hands thoroughly and remind her to do it before she breastfeeds, dresses or undresses the baby, washes or bathes it, after changing its diaper and disposing of the waste, after she has changed her own pads to catch the bloody vaginal discharge, after using the latrine, and before or after preparing food.
While you are washing your hands, ask the mother to start breastfeeding. (We will teach you the details of correct breastfeeding in the next study session). This will help you to check if there is any problem in breastfeeding and it helps to keep the baby calm during the assessment period. If the baby cries while you are assessing him or her it may give you inaccurate results for the assessment findings. Therefore, always try to keep babies calm while assessing them.
6.2 Screening the newborn for general danger signs
During the first home visit, the most important task is to screen all newborn babies for the presence of general danger signs in newborns (Box 6.1). These were already briefly listed in Study Session 1. Remember always to be vigilant, observant and gentle while assessing and managing a newborn baby, especially during the first few days of life. And always be alert to the potential presence of the key danger signs during the whole of the time you are with the mother and newborn.
Feeding problems are covered in detail in Study Session 7.
Box 6.1 General danger signs in newborns
- History of difficulty feeding, or unable to feed now; ask the mother about the baby’s feeding pattern.
- History of convulsion, or convulsing now; ask the mother, has the baby had any fits?
- Newborn seems lethargic or unconscious.
- Movement only when stimulated.
- Fast breathing.
- Severe lower chest in-drawing.
- Fever.
- Hypothermia (baby is cold to the touch).
- Baby developed yellowish discoloration before 24 hours of age; jaundice observed on the palms of the hands and soles of the feet.
- There is swelling of the eyes or eye discharge.
- Umbilicus is draining pus.
- More than 10 pustules (spots) are found on the skin.
6.2.1 How can you recognise a convulsion in a newborn?
![]() Apnoeia is pronounced ‘app-nee-ah’ and is a very dangerous sign. If you suspect that a newborn has had a convulsion, or you see signs of it during a visit, refer the mother and baby urgently to a higher level health facility.
Apnoeia is pronounced ‘app-nee-ah’ and is a very dangerous sign. If you suspect that a newborn has had a convulsion, or you see signs of it during a visit, refer the mother and baby urgently to a higher level health facility.
A convulsion (fit) in a newborn baby may present as:
- Twitching of part of the body (e.g. a hand), one side of the body, or the whole body (a generalised fit).
- Extension (spasm) of part of the body (e.g. an arm) or the whole body.
- Abnormal movements (e.g. mouthing movements, turning the eyes to one side or cycling movements of the legs).
- Apnoea (long periods without breathing).
It is often very difficult to recognise a convulsion in newborns because they usually do not have a generalised extension of the body and limbs, followed by jerking movements, as seen in convulsions in older children and adults. So it is very important to be alert for any unusual signs, even if they are not very obvious at first.
6.2.2 Is the newborn lethargic or unconscious?
An unconscious baby should be referred to a health facility immediately.
Look at the young newborn’s movements. Does it move less than you would expect from a normally active baby? Does the baby only move when stimulated to do so (is it lethargic)? If the mother has had a previous baby, or if there are other experienced mothers in the house, ask them if they think this baby is lethargic. It is a danger sign if it doesn’t seem to be moving or responding to stimuli normally.
6.2.3 Is the baby breathing too fast?
Urgently refer a newborn who appears to be in respiratory distress.
Count the baby’s breaths in one minute. Is it breathing normally or too fast? Fast breathing is a respiration rate equal to or greater than 60 breaths per minute. The normal breathing in a newborn is 40-60 breaths per minute, which you should check twice for one minute each time. Look for severe chest in-drawing: this means that while the baby is breathing in, the area of its lower ribs on each side ‘sucks’ inwards deeply (Figure 6.2).

6.2.4 Is the baby’s temperature normal?
Measure the baby’s temperature, preferably using a rectal thermometer inserted gently into the baby’s rectum through the anus, or use a normal thermometer held closely under the baby’s armpit (this is called the axillary temperature). Remember that the thermometer must be very clean before you use it. Wash it before and after use in clean water and then swab it with alcohol or another antiseptic solution. If you do not have a thermometer, use your hand to feel the baby’s head and body for fever, or low body temperature, by comparing how the baby feels with the temperature of your own or the mother’s skin.
![]() Refer a baby with a fever or hypothermia if its temperature does not return to normal quickly
Refer a baby with a fever or hypothermia if its temperature does not return to normal quickly
Fever is defined as a temperature equal to or greater than 37.5ºC. If you suspect that the baby may be too hot because it has been kept too warm by the mother, cool the baby by unwrapping its blankets and measure the temperature again after 15 minutes. If the temperature does not return to normal quickly, or if it is above 37.5ºC, refer the baby immediately. A high temperature is a danger sign for infection, which must be treated quickly. There is more on neonatal infections in Section 6.4 of this study session.

Hypothermia is defined as a temperature of equal to or less than 35.5ºC, but this is dangerously low for a newborn. If the baby feels chilled, don’t wait for its temperature to fall lower than 36.5ºC before taking fast action to warm it. Remove the clothes from its body and place it in skin-to-skin contact with the mother, between her breasts and inside her clothes (Figure 6.3). Wrap them both well with blankets, place a cap or shawl to cover the top and back of the baby’s head, and if the baby is not wearing socks, wrap its feet (this is called Kangaroo Mother Care, as you will see in Study Session 8.). If the baby’s temperature does not start rising towards normal within 30 minutes, or if it is below 35.5ºC, or the baby’s lips are blue, refer the baby immediately.
After assessing the newborn baby’s vital signs as described above, the next step is to assess for danger signs of newborn illnesses.
6.3 Does the baby have jaundice?
Signs of jaundice are a yellow discoloration of the skin and of the sclera (white of the eye). However the sclera is often difficult to see in newborns, so the skin colour is used to detect jaundice. First, ask the mother if she noticed any yellowish discoloration of the baby’s skin before it was 24 hours of age. Then look for yourself and also check if the palms of the baby’s hands and the soles of its feet are yellow. Jaundice is caused by excess deposits of a yellow pigment called bilirubin (the condition is also called hyperbilirubinaemia, ‘too much bilirubin’). It appears in the skin when too much haemoglobin (the oxygen-carrying protein) in the red blood cells is broken down, or when the liver is not functioning well and cannot deal with the bilirubin, or when the bile excretory duct is obstructed. (Bile is a substance produced by the bile gland which helps in the breakdown of bilirubin).
In untreated cases, the excess bilirubin will have serious effects on the newborn baby’s brain and can be fatal; if left untreated, it can have long-term neurological complications (complications related to abnormalities in the central nervous system, for example partial paralysis, growth retardation or learning difficulties).
6.4 Infection in the newborn
Infection is common in newborn babies and neonatal infection is one of the major causes of their deaths.
Can you remember (e.g. from Study Session 1) why there is a higher risk of infection in newborns than in older children or adults?
A key reason is the immaturity of the newborn’s immune system, which takes several months after birth to develop sufficiently to give much protection from infection.
PROM was the subject of Study Session 17 in the Antenatal Care Module; prolonged or obstructed labour was covered in Study Session 9 of the Labour and Delivery Care Module.
This means that newborns are especially vulnerable to exposure to infectious agents during pregnancy, delivery and in the home after the birth. The most common risk factors for newborn infection are prolonged premature rupture of the fetal membranes (PROM), prolonged labour or obstructed labour, and pre-existing lower genital tract infection in the mother. We first consider eye infections in newborns.
6.4.1 What are the signs of eye infection in newborns?
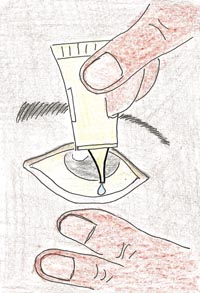
If a mother has the bacteria in her genital tract that cause sexually transmitted infections (particularly chlamydia or gonorrhoea), the germs can get into the baby’s eyes during delivery and may cause blindness. Look for swelling of the eyelids, redness of the inside part of the eye, or discharge from the eye. You can give prophylaxis (preventive treatment) immediately the baby is born by using tetracycline or another approved eye ointment, as shown in Figure 6.4. But if the newborn develops an eye infection in the postnatal period, you should refer him or her to the hospital or health centre for specialised assessment and treatment.
6.4.2 What are the signs of an infected umbilical cord stump?
![]() If any signs of an infected umbilical cord stump are present, refer the newborn to the hospital or health centre. Do not use antibiotic powder. Do not put aspirin or other home remedies on the cord.
If any signs of an infected umbilical cord stump are present, refer the newborn to the hospital or health centre. Do not use antibiotic powder. Do not put aspirin or other home remedies on the cord.
Look at the umbilicus: is it red or draining pus? Infection of the umbilical cord stump presents with the following danger signs:
- An offensively smelling cord with a discharge of pus.
- A cord that remains wet and soft and is not drying properly.
- Redness of the skin around the base of the cord.
With good preventative cord care, infection of the umbilical cord should not occur. Prevention consists of proper hand washing, good personal hygiene of the mother and the baby, using clean sterile thread to tie the cord and sterile instruments to cut it, and keeping the cord stump clean and dry.
6.4.3 What are the signs of skin infection?
The two common forms of skin infection in the newborn are:
If you find signs of impetigo or monilial rash you should refer the newborn to the hospital or health centre
- Impetigo caused by Staphylococcus bacteria in the skin, which presents as pus-filled blisters (pustules) usually seen around the umbilicus or in the nappy area. Are there many pustules? More than 10 is a general danger sign.
- Monilial rash is caused by a fungus (Candida or Monilia species). This almost always occurs in the nappy area and presents as red, slightly raised spots, and is most marked in the skin creases.
In contrast, a nappy rash due to irritation of the skin by stool and urine, usually affects the exposed areas of the skin and not the creases. Improved hygiene, washing the baby often with clean warm water and allowing the skin to dry completely, is usually enough to resolve nappy rash unless it becomes infected.
A sweat rash, due to excessive sweating, may look like a skin infection, but it is not. It presents as small, clear blisters on the forehead or a fine red rash on the neck and trunk. Reassure the mother that this is not a serious problem and advise her to wash the baby with warm water and prevent overheating.
6.4.4 What is neonatal tetanus?
![]() Refer a baby with signs of tetanus urgently to the nearest hospital or health centre. On the way protect the baby from hypothermia and give breast milk.
Refer a baby with signs of tetanus urgently to the nearest hospital or health centre. On the way protect the baby from hypothermia and give breast milk.
Tetanus in the newborn is caused by bacteria (Clostridium tetani) that infect dead tissues such as the umbilical cord stump. Tetanus bacteria are present in soil and animal dung, which may infect the cord or other wounds, for example during some harmful traditional practices. These bacteria produce a powerful toxin (poison) that affects the nervous system. Suspect tetanus if you observe the following signs in the newborn;
- Increased muscle tone (spasm), especially of the jaw muscles and abdomen.
- Generalised muscle spasms and convulsions, often precipitated by stimulation such as handling or loud noises. The baby may arch backwards during a spasm (Figure 6.5).
- Most babies with tetanus will develop severe breathing difficulty and even with good medical care many will die.

6.4.5 How can you prevent infection in newborns?
The best way of preventing infection is to deliver a baby at the health facility using clean and sterile instruments by skilled personnel. But this is often impossible in rural Ethiopia, where most births take place at home; so your role in reducing neonatal infection is absolutely vital. There are many simple ways in which infections can be prevented in newborns, and you should know a lot about them from the earlier study sessions in this Module:
- Avoid overcrowding at home and keep normal newborns with their mothers whenever possible. Do not separate mothers and their newborns unless absolutely necessary.
- Encourage breastfeeding. Breast milk contains antibodies, which help to protect the newborn from infections.
- Try to persuade the mother not to wash the baby for the first 24 hours after birth. Vernix (the curd or cheese-like secretion covering the newborn’s skin) has antibacterial properties and should be left to be absorbed by the baby’s skin.
- Always wash your hands thoroughly with soap before handling newborns. Hand washing is probably the most important method of preventing the spread of infection.
- Help the mother with her personal hygiene and cleanliness and try and ensure that the room where mother and baby live is clean.
- Always use sterile and clean instruments to cut the umbilical cord, and keep the stump clean and dry. Clean all instruments used for maternal and newborn care with alcohol before every examination.
- Remember that routine prophylactic eye care immediately after delivery with antibiotic ointment (tetracycline) prevents eye infection, but you should use it only once.
- Don't forget immunization: all pregnant women should be vaccinated with at least two doses (and preferably up to five doses) of tetanus toxoid to prevent neonatal tetanus.
6.5 Neonatal assessment check list for critical conditions
After asking the mother about any neonatal problems and doing the basic assessment and examination yourself, you can classify the newborn baby based on the following assessment check list (Table 6.1).
After assessing the baby for critical conditions, remember to check again for any gross signs of congenital anomaly and/or gross signs of birth trauma (e.g. defects on the back, swelling of the head, excessive bruises), which can be a cause of acute blood loss leading to anaemia.
In Study Session 7 we will describe everything that you and the new mother need to know about breastfeeding. Checking that the baby is feeding well and that the mother is managing to breastfeed adequately is part of every postnatal visit. You should also weigh the baby at every visit to make sure that it is gaining weight normally. This is particularly important for babies who were not born at term (37 to 42 weeks of gestation), or whose birth weight was below the normal range (equal to or greater than 2,500 gm).
Preterm babies (born at 32 to 36 weeks gestation), very preterm babies (less than 32 weeks of gestation), and those who are low birth weight (1,500 to under 2,500 gms) or very low birth weight (less than 1,500 gms) may have serious additional problems because coordination of swallowing and breathing is not well established, so they cannot feed properly. You will learn all about special care for these tiny babies in Study Session 8.
| Ask and check | Classify | Action taken |
|---|---|---|
| If there is any one of the general danger signs, classify as: POSSIBLE SERIOUS INFECTION | Refer URGENTLY to hospital or health centre. Keep the newborn baby warm and give him or her breast milk on the way. |
| If there is any one of these danger signs, classify as: POSSIBLE INFECTION OR JAUNDICE | Refer URGENTLY to hospital or health centre Keep the newborn baby warm and give him or her breast milk on the way. |
NORMAL BABY | Breastfeeding and care to prevent infection and keep the baby warm. |
Summary of Study Session 6
In Study Session 6 you have learned that:
- A key part of every postnatal visit is to assess the newborn for general danger signs, including: not feeding, convulsions, lethargy or abnormal body movements, fast breathing with chest in-drawing, jaundice, skin lesions including umbilical infection, eye discharge and neonatal tetanus.
- Routine preparations before assessing the newborn are to wash your hands thoroughly and ask the mother to begin breastfeeding, so you can assess how well the baby feeds, and also to keep the baby calm during your assessment.
- Asking the mother about her newborn baby’s condition is an important source of information in making your assessment.
- Make sure that you explain to her the ways in which she can help to prevent infection in her newborn, including hand washing, keeping the baby clean and the cord stump clean and dry, and avoiding overcrowding or unhygienic conditions where they are living.
- According to the ‘Assess and Classify Chart’ (Table 6.1), the possible classifications are: Possible serious infection, possible infection or jaundice, or a normal baby. Classification helps you to make the proper decision about what action to take.
Self-Assessment Questions (SAQs) for Study Session 6
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
First read Case Study 6.1 and then answer the questions that follow it.
Case Study 6.1 Postnatal assessment of a female newborn
A female baby was delivered by a 32 year-old mother at a gestational age of 39 weeks. You assess the baby at 28 hours after the birth. She has a birth weight of 3,000 gm and presented with a history of convulsion, no feeding at all and a body temperature of 38.5°C.
SAQ 6.1 (tests Learning Outcomes 6.1 and 6.3)
- a.How do you classify this baby based on her gestational age?
- b.How do you classify her according to her birth weight?
- c.List the general danger signs present in this newborn.
- d.What is your comment on the body temperature of this baby?
- e.What will be your final classification of this newborn baby and how should you manage her condition?
Answer
- a.At 39 weeks of gestation, this baby is classified as a normal term baby.
- b.The birth weight is 3,000 gm, which is classified as a normal birth weight.
- c.The general danger signs are no feeding, history of convulsions, and high temperature.
- d.The temperature (38.5˚C) is abnormal and the newborn has a fever. The normal temperature of a newborn is above 36.5 to below 37.5˚C.
- e.This baby has three major danger signs (no feeding, convulsion and fever) and is classified as a possible infection. Your management of this baby should be an urgent referral to a hospital or health centre, with advice to keep her warm and feed breast milk on the way.
Now read Case Study 6.2 and answer the questions that follow it.
Case Study 6.2 Postnatal assessment of a male newborn
You assess an eight hour-old male newborn who was delivered by a 27 year-old first-time mother at a gestational age of 31 weeks. He had a birth weight of 1,300 gm, and presented with a respiratory rate of 72 breaths per minute and chest in-drawing. His body temperature is 34.5°C.
SAQ 6.2 (tests Learning Outcomes 6.1 and 6.3)
- a.How do you classify this baby’s gestational age?
- b.How do you classify him according to his birth weight?
- c.Is the respiratory rate of 72 breaths per minute normal or not? What is the normal range of respiration?
- d.What about the temperature of this newborn? Is it normal?
- e.What should your management of this newborn be?
Answer
- A.As the baby was born at 31 weeks of gestation, he is classified as a very preterm baby.
- B.The birth weight is 1,300 gm, so he is classified as very low birth weight.
- C.His respiration rate of 72 breaths per minute breathing is abnormal. This newborn has fast breathing. The normal breathing rate of the newborn is 40-60 breaths per minute.
- D.The temperature (34.5˚C) is abnormally low; the newborn has hypothermia. The normal temperature of the newborn is above 36.5˚C to below 37.5˚C.
- E.As he is a very preterm and very low birth weight baby, with two major danger signs (fast breathing and hypothermia), he is classified as possible infection. The management should be an urgent referral to a hospital or health centre, with advice to keep him warm and feed breast milk on the way.
SAQ 6.3 (tests Learning Outcomes 6.1, 6.2 and 6.4)
Imagine it is your first visit to a new mother who had a normal birth. You are assessing that her newborn baby is OK, including checking for signs of infection.
- What would you ask her before commencing your examination of the baby?
- What would you be sure to look for/check when you examine the baby?
Use Table 6.2 below to help you to organise your answers.
| Questions to ask the mother | Things to look for/check in the newborn |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Answer
| Questions to ask the mother | Things to look for/check in the newborn |
|---|---|
| Is the mother remembering to wash her hands before breastfeeding, and keeping the baby and herself clean? | Do the mother and baby look clean and well? Is the room clean and well kept? |
| Has she noticed any unusual movements, spasms, of an arm or the whole body? | If yes, observe carefully to see if the baby may be suffering from convulsions. |
| Is her baby breathing steadily and without effort? | If the mother is worried, check for chest in-drawing (the baby’s chest sucking inwards deeply at the lower ribs); also check for any signs of convulsions. |
| Is the mother taking care to keep the umbilical cord stump clean and dry? Has she noticed any ‘smelliness’ from the umbilical cord? | See if there is discharge, or redness of the skin around the base of the cord. Remind the mother about the importance of keeping it clean and dry. |
| Has she noticed any redness or discharge from the baby’s eyes? | Was tetracycline (or another approved eye ointment) applied at birth? |
| Does the baby seem too hot, or too cool? | If the baby seems hot take it’s temperature (with a sterile and clean thermometer), but also check if she has it too well wrapped up. If it is cold, check for hypothermia. |
| Does the mother have any problems with breastfeeding? | If yes, check the mother for cracked nipples, or heat in the breast (mastitis or an abscess). If reluctant to breastfeed, remind her how important breast milk is as nourishment for her baby and protecting it from infection. |
| Does the baby have any signs of a rash? | If yes, is it just nappy rash or sweat rash, or are there any pustules (pus filled blisters)? If so, are there more than 10? |
| Did she or the baby go through any harmful traditional practices following the birth? | If yes, check the baby for any signs of tetanus (e.g. muscle spasms) and ask if the mother has been immunized against tetanus. |
| Does she feel well generally? Is she coping with looking after a new baby? | Is the mother getting enough support and is the baby getting all the care it needs? |
