Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 21 November 2025, 7:02 AM
Postnatal Care Module: 7. Breastfeeding, the Warm Chain Principle and Counselling HIV-Positive Mothers
Study Session 7 Breastfeeding, the Warm Chain Principle and Counselling HIV-Positive Mothers
Introduction
During the postnatal period, counselling the mother of a normal healthy newborn baby focuses on many issues, including those already covered in earlier study sessions, such as infection prevention, nutrition for the mother, and family planning. In this study session, we return in detail to two topics that have been touched on previously: how to begin and maintain optimum breastfeeding, and how to keep the baby warm using the ‘warm chain principle’. The first part of this study session is about feeding the normal weight, healthy, full-term baby. Then we will look at the special counselling that HIV-positive mothers need about feeding babies who are full term and normal weight. Study Session 8 will cover the special care needed to feed and maintain the body temperature of preterm or low birth weight babies.
Learning Outcomes for Study Session 7
When you have studied this session, you should be able to:
7.1 Define and use correctly all of the key words printed in bold. (SAQ 7.2)
7.2 Explain the benefits of breast milk for the newborn and the advantages of exclusive breastfeeding for the mother and newborn. (SAQ 7.1)
7.3 Describe the steps in establishing optimum breastfeeding through good positioning of the mother and good attachment of the baby to the breast. (SAQ 7.2)
7.4 Describe how to counsel the mother who is HIV-positive on feeding options for her baby to reduce the risk of transmitting HIV through breast milk. (SAQ 7.1)
7.5 Describe how newborns lose heat and how to prevent hypothermia by using the ‘warm chain principle’. (SAQ 7.3)
7.1 Counselling the mother on newborn feeding
It is always advisable to provide counselling about newborn feeding during the antenatal period and continue reinforcing it during the postnatal period. This teaching should focus on establishing and maintaining optimum breastfeeding. The criteria for achieving this are summarised in Box 7.1.
Box 7.1 Optimum breastfeeding criteria
- Initiation of breastfeeding within one hour after birth (early breastfeeding).
- Nothing is given to the baby other than breast milk for the first six months (exclusive breastfeeding).
- Colostrum is not thrown away. It is rich in protein and antibodies and is useful to the newborn; you should tell the mother to feed it to her newborn, because it is the first ‘immunization’ that her baby will get.
- The mother is sitting in a good position while breastfeeding.
- The baby has good attachment to the breast while breastfeeding.
- There is effective suckling.
When you arrive for a postnatal visit, ask the mother to put the baby to the breast to check for good positioning and good attachment (we describe how you do this below). If the baby was fed recently, wait for at least an hour before putting him or her back to the breast. This will allow you to observe how the baby is breastfeeding and identify if there are any breastfeeding problems, which you can help the mother to overcome. Before you leave the house, ensure the mother understands how to breastfeed her baby optimally.
7.1.1 Four signs of good positioning
To begin with, the mother should sit comfortably (see Figure 7.1a), maintaining the four signs of good positioning:
- with the newborn’s head and body straight
- facing her breast, with baby’s nose opposite her nipple
- with the newborn’s body close to her body
- supporting the baby’s whole body, not just the neck and shoulders.
If the mother has had a caesarean delivery, or her abdomen is sore for some other reason, she may be more comfortable supporting the baby as shown in Figure 7.1(b). It keeps the baby’s weight off her abdomen. She can feed twins this way too, with one on each breast. At night, or if she is tired and needs to rest, she can feed the baby while lying down (Figure 7.1c), but only if she stays awake.
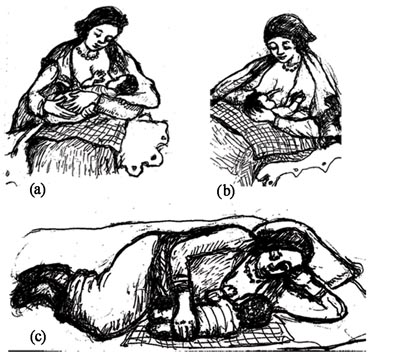
Giving breastfeeding in the lying down position (Figure 7.1c) is not advisable unless the mother is awake. Can you suggest why not?
If the mother is falling asleep she may roll onto the newborn, who may be unable to breathe and asphyxiate (die from lack of oxygen).
7.1.2 Four signs of good attachment
Once good positioning is established, show the mother how to help the newborn to attach to the nipple. She should:
- Touch her newborn’s lips with her nipple
- Wait until her newborn’s mouth is opening wide
- Move her newborn quickly onto her breast, aiming the newborn’s lower lip well below the nipple. Then check for signs of good attachment (see Figure 7.2).
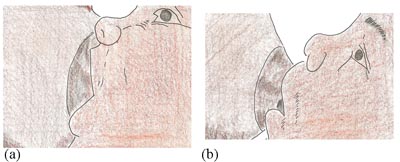
The four signs of good attachment are:
- Mouth widely opened
- Lower lip turned upward
- Chin touching the breast
- More of the areola (the dark ring around the nipple) is seen above the baby’s mouth than below it.
Advise the mother to empty one breast before switching to the other, so that the newborn gets the nutrient-rich hind milk (last milk), which is produced when the breast is almost empty.
7.1.3 Effective suckling
Good signs of effective suckling are if the newborn takes slow, regular and deep sucks, sometimes pausing. The mother should tell you that she is comfortable and pain free.
If you observe that the attachment and suckling are inadequate, ask the mother to try again and reassess how well the baby is feeding. If they still cannot establish optimum breastfeeding, then you should assume that the newborn has a feeding problem and/or the mother has breast problems that make attachment difficult. If so refer the baby and the mother to a health facility for further advice and care.
7.2 What are the benefits of breastfeeding?
Breastfeeding provides many benefits to both the newborn and mother. You should encourage mothers to breastfeed exclusively for at least the first six months by explaining the benefits to them.
7.2.1 Benefits to the newborn of breastfeeding
Breast milk is the ideal feed for full term newborns as it provides all the nutrients in the correct amount and proportion for normal growth and development until the age of six months. It is easily digested and absorbed. Also, breast milk is clean and warm, and avoids the dangers of feeding formula milk which comes as a powder and has to be made up with water and fed in a bottle.
Can you suggest the sources of risk to the newborn from badly made formula milk?
There is a risk of infection from making the milk with contaminated water, or if the bottles and teats are not properly sterilised. If the mother makes several feeds at one time, and she cannot keep them cold because she has no refrigeration facilities, bacteria may grow in the warm milk. Also, if she puts too little or too much milk powder in each bottle, the baby will suffer from malnourishment if the formula is too weak, or it will get an excessive load on its organs from too concentrated formula.
Breast milk contains many anti-infective factors, such as antibodies, living cells and molecules that help the baby's body to fight infection. It also encourages the growth of beneficial bacteria in the newborn's bowel. These properties of breast milk help to prevent diarrhoeal diseases, the major cause of death of newborns in poor communities.
Breast milk also decreases the risk of allergy in the newborn. Allergies are adverse reactions of the body against components of the diet, pollen from plants, animals and other harmless things that touch the body or get into it through the nose, mouth or eyes. Newborns are more at risk of allergies if there is a strong family history of allergy.
7.2.2 Benefits to the mother of breastfeeding
Breastfeeding is (almost) free – the mother needs additional food while she is breastfeeding, but the cost is much cheaper than buying formula feeds, bottles and teats. It is instantly available at all times, so the mother does not have the trouble of sterilising bottles and teats, and preparing formula feeds many times every day. It is emotionally satisfying for the mother to successfully breastfeed her baby and the close contact helps to form a strong bond between mother and newborn.
The hormone (oxytocin) that triggers the milk to spurt from the breast by contracting the tiny muscles around the nipple, also makes the muscles in the uterus contract. So breastfeeding helps the uterus to return to its normal size.
What other benefit can you suggest results from the contractions of the myometrieum (the muscle layer in the uterus) during breastfeeding?
The contractions help to close the torn blood vessels where the placenta detached from the uterine wall, and this reduces the amount of normal vaginal bleeding during the puerperium, and decreases the risk of postpartum haemorrhage.
Breastfeeding helps the mother to lose excessive weight if she gained too much during the pregnancy. Pregnancy, not breastfeeding, alters the shape of a woman’s breasts.
7.2.3 Breastfeeding and birth control
Exclusive breastfeeding (feeding only breast milk to the baby and no other fluids or foods) greatly reduces the chance of the mother becoming pregnant again if it is begun early (within an hour of the birth), and maintained for the recommended first six months. Explain to the mother and her partner that if a woman has sex and is not exclusively breastfeeding, she can become pregnant as soon as four weeks after delivery. Therefore, information on when to start a contraceptive method will vary depending on whether the woman is breastfeeding or not.
In Ethiopia it is recommended that you try to convince mothers to put their babies on exclusive breastfeeding for six months for many reasons, including that it will suppress her menstrual cycle, but only if she fulfills the following criteria:
- The baby should be exclusively breastfed on demand (whenever the baby wants to be fed) a minimum of 8-12 times a day, including at least one feed during the night.
- The interval between daytime feeds should not be more than four hours apart and night feeds should not be more than six hours apart.
- If her menstrual periods return even while she is exclusively breastfeeding, she could easily become pregnant!
Emphasise that after six months, she will not be protected from becoming pregnant by breastfeeding alone. She should choose another family planning method. You will learn all about this in the Module on Family Planning in this curriculum. Table 7.1 summarises the benefits to the mother and the newborn of exclusive breastfeeding.
| Mother | Newborn |
|---|---|
| It is much cheaper than formula | It is fully nutritious |
| Always available (ready) | Easily digested and absorbed |
| Mental satisfaction | It is clean and warm |
| Reduced bleeding | It contains anti-infective substances |
| Can be used as birth control | Prevents diarrhoeal disease |
| Helps lose excessive weight | Decreases allergy risk |
| Increases bonding with the newborn | Increases bonding with the mother |
7.3 Counselling the HIV-positive mother about feeding her baby
HIV-testing and counselling and PMTCT is covered in detail in the Communicable Diseases Module, and also in the Antenatal Care Module.
Mothers who are HIV-positive and their babies need special care before, during and after labour and delivery. Therefore, if the mother is counselled and HIV-tested before or during pregnancy, and she knows that she is HIV-positive, you should try to convince her to deliver her baby in a health facility. That way she and her baby will get special care from health professionals with special training in delivering babies from HIV-positive mothers, and preventing maternal to child transmission (PMTCT of HIV).
In the postnatal period, she may need to take antiretroviral (ARV) drugs prescribed for her by the HIV clinic, and your support is vital in helping her to keep to her drug regimen. Maintain confidentiality about her status and conduct frequent visits to this woman as she may require a lot of psycho-social support immediately after the delivery. If it is available link her with the community social support group. Always make sure her partner is counselled and HIV-tested and also involved in the whole care process.
7.3.1 Breast milk or formula?
In this study session our focus is on the risk of HIV being transmitted from the mother to her newborn baby in her breast milk, and how you can support and counsel her about feeding options. If 20 HIV-positive mothers breastfeed their HIV-negative babies exclusively for the first six months, on average one to three of the babies will become infected with HIV through its mother’s breast milk. So the mother has a difficult choice to make. She has to balance the risk to her baby from HIV transmission during breastfeeding, against the risk of not breastfeeding and losing all the benefits described above. Formula feeding also exposes the baby to increased risk of infection from unsterilised bottles and malnutrition from incorrectly made feeds.
7.3.2 Replacement feeding and the AFASS criteria
Exclusive breastfeeding is NOT recommended for the babies of HIV-positive women, since the only way to protect the baby completely from HIV transmission from its mother is to feed it on formula milk. This is known as replacement feeding. However, many families cannot afford to buy milk formula to feed the baby, and bottle feeding may be socially unacceptable in some communities. With all these issues in mind the World Health Organisation (WHO) has set the following criteria (known as the AFASS criteria), which need to be met before counselling an HIV-positive mother to use formula milk:
- Acceptable: Replacement feeding for breast milk is acceptable by the mother, the family and others who are close to the family.
- Feasible: The mother has access to clean and safe water for cleaning the feeding bottles, teats, measuring cup and spoon, and diluting the formula milk if it comes as a powder.
- Affordable: The family can afford to buy enough formula milk or animal milk to feed the baby adequately.
- Sustainable: The mother is able to prepare feeds for the child as frequently as recommended and as the baby demands.
- Safe: The formula milk should be safe and nutritious for the health of the baby.
The AFASS criteria are illustrated in Figure 7.4. When replacement feeding fulfils the AFASS criteria, avoidance of all breastfeeding by HIV-positive mothers is recommended.
7.3.3 Reducing the HIV risk from breastfeeding
If replacement feeding is rejected by the HIV-positive mother, for whatever reasons, there are some things that she can do to reduce the risk of HIV transmission during breastfeeding. Counsel her to:
- Keep the intervals between breast feeds as short as possible (no longer than three hours) to avoid accumulation of the virus in her breast milk.
- If she develops a bacterial infection (mastitis) of the breast, or she has a cracked nipple, stop feeding from the infected breast and seek urgent treatment.
- Check the infant’s mouth for sores and seek treatment if necessary.
- Make a transition to replacement feeding if her circumstances change and she can meet the AFASS criteria.
At six months, if replacement feeding is still not acceptable, feasible, affordable, sustainable and safe, counsel her to continue breastfeeding, but with additional complementary foods. All breastfeeding should stop once a nutritionally adequate and safe diet without breast milk can be provided.
7.4 Keeping the baby warm
Newborn babies cool down or heat up much quicker than older children or adults because they cannot regulate their body temperature as easily. They are particularly vulnerable to hypothermia, which means excessive cooling of the baby, so the body temperature falls below 35.5oC measured in the baby’s armpit (or use a rectal thermometer). If this low temperature continues even for a short time, it will cause the baby’s body systems to stop functioning properly and this is life-threatening. Hypothermia is a major cause of morbidity and mortality in a newborn baby, particularly pre-term babies (born before 36 weeks of gestation) and those with low birth weight (below 2,500 gm). Study Session 8 will teach you all about the problems and management of these early or tiny babies.
Hypothermia is usually caused more by the mother’s lack of knowledge rather than lack of covers and clothes to keep the baby warm. So make sure you explain to the mother the importance of keeping the baby warm all the time to ensure that a normal body temperature of above 36.5°C and below 37.5°C can be maintained.
7.4.1 How to take the newborn’s temperature
Place the thermometer in the newborn's armpit (or rectum if you have a rectal thermometer) for two to three minutes, then read the temperature according to the type of thermometer you have. (You learned how to use different types of thermometer in Study Session 9 of the Antenatal Care Module.) Thermometers should be stored dry when not in use. Before and after you take anyone’s temperature, the thermometer should be cleaned with antiseptic to prevent carrying infection from one person to another. It is important to notice when the temperature is even a little bit lower than normal, before it reaches as low as 35.5oC.
7.4.2 When are newborns at greatest risk of hypothermia?
Newborns that have particular problems in producing enough heat in their bodies, or who lose too much heat because of poor care by the mother, are at the greatest risk.
Newborns who may not produce enough heat include those who are:
- Preterm
- Underweight for gestational age
- Wasted (thin)
- Infected
- Hypoxic (starved of oxygen during labour and delivery).
Newborns that lose too much heat include those who are:
- Wet after washing, or left in wet clothes
- Have not been fed enough
- Exposed to a cold environment, not enough clothes or covers, especially when they are sleeping
- Naked when they are breastfed
- Fed close to a cold window, in a draught of cold air.
7.4.3 How do newborns lose heat?
The mechanisms of how the newborn loses heat are summarised in Figure 7.5, and described below.
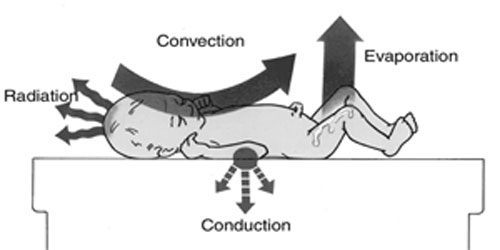
Convection. This is the loss of heat from the newborn's skin to the surrounding air. Newborns lose a lot of heat by convection when exposed to cold air or draughts.
Conduction. This is the loss of heat when the newborn lies on a cold surface. Newborns lose heat by conduction when placed naked on a cold table, weighing scale or are wrapped in a cold blanket or towel.
Evaporation. This is the loss of heat from a newborn's wet skin to the surrounding air. Newborns lose heat by evaporation after delivery or after a bath. Even a newborn in a wet nappy can lose heat by evaporation.
Radiation. This is the loss of heat from a newborn's skin to distant cold objects, such as a cold window or wall etc.
Finally, knowing that the newborn can lose heat by the four mechanisms described above, you should counsel the mother to avoid exposing the baby to drafts. Counsel her that before she removes the baby's clothes for a bath, close all doors and windows; cover the wet baby and dry him or her quickly.
Stop reading for a moment and think of your own experience in your community. Have you seen situations when mothers were in danger of letting their baby lose heat in any of the ways described above?
7.4.4 The warm chain principle in postnatal care
The mother should understand that keeping the baby warm is not a one-time job; it is rather a continuous job which means adhering to the warm chain principle. A warm chain is a system of keeping a baby warm immediately after delivery, wherever it occurs (at a health facility or the mother’s home), during transportation and while feeding and caring for the baby. The components of the warm chain are listed in Box 7.2.
Box 7.2 Components of the warm chain
- Drying and wrapping the baby immediately at birth.
- Keeping the baby warm during any procedure, including resuscitation.
- Keeping the immediate newborn in skin-to-skin contact with the mother.
- Early initiation of breastfeeding within one hour of the birth; the warm milk and contact with the mother's body helps to keep the newborn baby warm.
- Postponing bathing the newborn for the first 24 hours.
- Keeping the baby warm during transportation.
- Dressing the baby in appropriate clothing and bedding at all times.
The warm chain principle has to be maintained for all babies, but special care should be taken to keep preterm and low birth weight babies warm, as you will see in the next study session.
Summary of Study Session 7
In Study Session 7 you have learned that:
- You have an important role in the postnatal period in counselling the mother on breastfeeding and how to keep the baby warm.
- You should teach the mother about the different positions for optimum breastfeeding and the signs of good attachment.
- There are many benefits of breast milk and breastfeeding for the mother and her newborn, compared to formula milk, including reduced risk of gastrointestinal infection in the baby, and faster contraction of the uterus.
- HIV-positive mothers should be counselled to avoid breastfeeding completely if they can provide replacement feeding with formula milk which fulfils the AFASS criteria: acceptable, feasible, affordable, sustainable and safe.
- Newborns can lose heat rapidly through conduction, convection, evaporation and radiation; the warm chain principle tells you how to keep the baby warm at all times.
Self-Assessment Questions (SAQs) for Study Session 7
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 7.1 (tests Learning Outcome 7.2 and 7.4)
You are wondering what to say to an HIV-positive mother who is particularly keen on breastfeeding. How would you advise her?
Answer
There are many ways in which you might have made notes on this difficult situation. You would have sympathised with the mother’s wish to breastfeed and probably pointed out the benefits for the baby (e.g. protection from infection, correct nutrients, reduction in risk of allergy), and the benefits for the mother (breast milk is cheaper, breastfeeding helps the uterus to contract, it is useful for birth control, etc). But you would also have told her of the risk of transmitting HIV to the baby via breastfeeding.
When you discuss formula feed as the alternative you would have explained the critical importance of clean water, and proper sterilisation of the bottles and teats, as well as the need to measure everything accurately so the baby gets the correct nourishment.
Then you would go through the AFASS criteria and the questions in Figure 7.4. If she answered ‘yes’ to them all, you would encourage her to use formula or animal milk, and also counselled her about birth control. If she answered ‘no’ and she really wants to breastfeed, you would have explained how she can reduce the risk of HIV transmission by feeding at very short intervals (no longer than three hours), and stop feeding from a breast that has a cracked nipple. You should have reminded her to check the baby’s mouth for sores, and seek urgent treatment for herself and her baby if either of them feels ill.
SAQ 7.2 (tests Learning Outcome 7.2)
Which of the following definitions is incorrect? In each case, give the correct definition.
A Exclusive breastfeeding is only feeding one baby at a time.
B Good positioning for breastfeeding is when the mother is sitting comfortably.
C Good attachment means the baby has ‘a good mouthful of breast’.
D Early breastfeeding requires the mother to get up around dawn for the first feed.
E The principle of the warm chain means that you pay attention to keeping the baby warm at all times, so as to avoid hypothermia.
Answer
A False: Exclusive breastfeeding is giving nothing to the baby other than breast milk for the first six months.
B True. But look back to Section 7.1.1 and check you are clear about how to maintain the mother in good positioning.
C True: Look back to Section 7.1.2 and check you remember precisely the four signs of good attachment.
D False: Early breastfeeding is initiation of breastfeeding within one hour after birth.
E True: The warm chain principle means taking action to keep the baby warm at all times.
SAQ 7.3 (tests Learning Outcome 7.5)
You are visiting a new mother and you notice that the baby feels very cold. You are worried about hypothermia. What do you do?
Answer
- Place the baby in skin-to-skin contact with the mother, wrap them both in warm blankets, put a cap or shawl on the baby’s head and put its socks on or wrap its feet.
- Take the baby’s temperature and if it is less than 37.5oC take it again after half an hour. If its temperature is not beginning to rise fairly soon, refer the baby urgently.
- While you are waiting to see if the baby is getting warmer, check for a simple explanation for why the baby is cold. Ask the mother if the baby has been recently wet, or has not been recently fed, or whether she feeds it naked. Check if the room has open windows or the baby is in a cold draft of air.
- Explain to the mother how newborns lose heat (the key ways are summarised in Section 7.4.3) and tell her why it is important always to keep the baby warm.
- Talk her through the components of the ‘warm chain’. If you can’t remember this look again at Box 7.2.