Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 5 February 2026, 9:09 AM
Antenatal Care Module: 5. Fertilisation, Implantation and the Fetal and Placental Circulation
Study Session 5 Fertilisation, Implantation and the Fetal and Placental Circulation
Introduction
The exact moment when a fertilised ovum, embryo, fetus or baby is called a ‘human being’ is controversial, and differs between individuals, religious groups, legal systems and nations. We will not address this difficult concept in this study session, but focus instead on the theoretical knowledge of how fertilisation and implantation of the ovum in the uterus occurs, and how the fetus is nourished as it develops during the nine months of gestation. This study session will also help you to recognise factors affecting fetal development that may lead to complications during the antenatal period.
Learning Outcomes for Study Session 5
When you have studied this session, you should be able to:
5.1 Define and use correctly all of the key words printed in bold. (SAQ 5.1)
5.2 Describe the process of fertilisation, implantation of the fertilised ovum in the uterus, and the early development of the embryo and the placenta. (SAQs 5.1 and 5.2)
5.3 Explain how the fetal circulation functions and how the fetus gets nutrition from the mother via the placenta. (SAQs 5.1 and 5.3)
5.1 Male and female sex cells
Before we look at the fertilisation process in humans, you need to understand the structure of both male sperm and female ova.
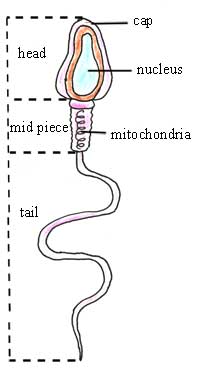
5.1.1 Sperm: the male sex cells
The mature sperm cell (see Figure 5.1) is a little swimming male sex cell. It consists of a head, body and tail. The head is covered by a cap and contains a nucleus of dense genetic material. It is attached to a region containing mitochondria, which supply the energy for the sperm’s activity. The tail is able to contract and relax, producing a characteristic wave-like movement.
Look at Figure 5.1. Can you explain how sperm move up the vagina, into the uterus and along the fallopian tubes?
A sperm has a tail that can wave about, propelling the sperm along as the tail ‘whips’ from side to side. As you probably remember from high school biology, the mitochondria are the energy-producing ‘motors’ in a cell, which supply the sperm tail with the energy for its movement.
The sperm make up only about 5% of what a man ejaculates during the sex act. This represents about 100 to 400 million sperm each time, carried in a nutritious fluid (semen) which helps to keep them alive. Sperm are very, very small in size; in fact, a single sperm is the smallest cell in the male body.
From puberty onwards, new sperm develop in the testes (testicles) throughout a man’s adult life. It takes about 72 days for one sperm to develop to maturity. Sperm production requires a temperature which is 3 to 5°C below body temperature — which is why the testicles are outside the abdomen, where they can remain a little cooler. Exposure of the testicles to a higher temperature will inhibit sperm production and may lead to infertility.
5.1.2 Ova: the female sex cells
As you learned in Study Session 3, a baby girl is born with all the ova that she will have in her lifetime, but they are in an immature state. Each ovum is a large cell, with an external cell membrane, and is full of liquid which is rich in protein. It has a nucleus which contains the female genetic material.
The ova are stored in ovarian follicles in the ovaries, and a few begin to mature each month after a girl reaches puberty at about 12 to 15 years of age. This process continues until the menopause at about age 48 to 50 years, when the menstrual cycles end.
Which hormones are involved in stimulating the maturation of ova?
The hypothalamus in the brain produces gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland (also in the brain) to produce follicle-stimulating hormone (FSH) and leutenizing hormone (LH). These two hormones act on the ovarian follicles and cause a few of the immature ova to begin maturation.
If the first day of the last menstrual period is called ‘day 1’, after how many days will a mature ovum be released from one of the ovaries?
Ovulation occurs at around day 14 of the cycle in most women.
5.2 Fertilisation
Fertilisation is defined as the fusion of the sperm nucleus with the ovum nucleus. For fertilisation to occur, sperm must be deposited in the vagina no earlier than three days before ovulation or within one day after ovulation. This short ‘window of opportunity’ is because the sperm and the ovum have only limited lives, and they both soon die if they do not meet and fuse in this period. Following ovulation, the ovum is picked up by the fimbriae of the fallopian tube on the same side of the body as the ovary that released the ovum. The ovum will remain in the fallopian tube, alive and fully functioning, for only about 12 to 24 hours. Sperm can live longer in the female reproductive system, up to 72 hours, but most die before this time.
Once deposited within the vagina, the sperm swim through the cervix and into the uterus, and then up into the fallopian tubes (look back at Figure 3.3 to remind yourself of the anatomy). Fertilisation of the ovum occurs in the fallopian tube. The movement of sperm on this long journey is helped by muscular contraction of the walls of the uterus and the fallopian tubes. Sperm can swim several millimetres (mm) in a second, so it only takes them about 15 minutes to get into the fallopian tubes, but millions die along the way.
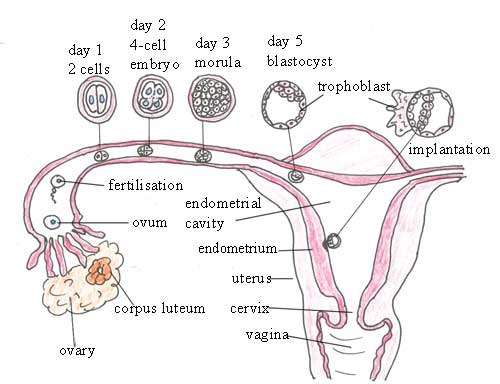
Only one sperm will succeed in fertilising the ovum (Figure 5.2), by penetrating its cell membrane and depositing the male genetic material into the female cell, where the two nuclei fuse. The fertilised ovum (zygote) immediately becomes resistant to penetration by any other sperm arriving later. After fertilisation occurs, the zygote remains in the fallopian tube for about 72 hours, and during this time it develops rapidly, as you will see in the next section.
5.3 Early development of the embryo
From the moment of fertilisation until the eighth week of pregnancy, the developing human is called an embryo. First it divides into two cells; then they each divide again to give four cells (see Figure 5.3). The process of cell division is repeated many times until a solid ball of cells called a morula is produced after about three days. As the cells in the morula continue to divide, they begin to move towards the outer edges of the ball, until it becomes a hollow ball of cells called the blastocyst at about five days after fertilisation. Notice in Figure 5.3 that the blastocyst has a solid mass of cells on one side of the cavity.
Morula is prounounced ‘morr you lah’. Blastocyst is prounounced ‘blass toh sist’.
While these changes are taking place in the early embryo, it is moving along the fallopian tube towards the uterus. This takes five to seven days.
5.3.1 Implantation
Between five to seven days after fertilisation, the blastocyst reaches the uterus and embeds itself in the thickened endometrium (lining of the uterus). This process is called implantation, and if the embryo survives it is the beginning of a pregnancy. However, the embryo may not implant, or it may not survive for more than a few days. In this case, it is shed from the uterus as the endometrium breaks down, and it passes out of the vagina in the menstrual fluid. The loss of a very early pregnancy in this way is very common, and the woman does not even know that she was momentarily pregnant.
![]() If you suspect an ectopic pregnancy, refer the woman immediately.
If you suspect an ectopic pregnancy, refer the woman immediately.
Implantation may also occasionally occur in the fallopian tube, which is called an ectopic pregnancy and is very dangerous for the woman. The tube may rupture as the embryo grows, and cause severe pain and loss of blood into the abdominal cavity.
If the blastocyst implants successfully in the uterus, the cells go on multiplying by cell division and moving around into new locations to form two distinct structures:
- Three or four blastocyst cells develop into the inner cell mass, which — over the next few weeks — will form into the recognisable structures of a human embryo, with a head, beating heart and tiny limbs. Some of these cells also develop into the fetal membranes that form a fluid-filled protective ‘bag’ around the embryo.
- The remaining 100 or so blastocyst cells form a structure called the trophoblast, which will provide the baby’s contribution to the placenta. The first stage of development of the placenta is when the trophoblast cells burrow into the endometrium.
Box 5.1 summarises the names and dates of the key stages in the development of a human, from fertilisation until one year after birth.
Box 5.1 Human developmental stages after fertilisation
Fertilisation: fusion of ovum and sperm on day one
Morula: solid ball of cells after three days
Blastocyst: hollow ball of cells after five days
Trophoblast: forms early embryo, fetal membranes and placenta after five to seven days
Embryo: the developing human from fertilisation to the eighth week of pregnancy
Fetus: the developing human from nine weeks of pregnancy to birth at around 40 weeks
Neonate: newborn baby from birth to 28 days old
Infant: baby or young child aged less than one year.
5.4 The placenta
The placenta is a temporary organ required for the development of the embryo and fetus. It allows for the exchange of nutrients and oxygen from mother to fetus, and the transfer of fetal waste products back to the mother for disposal by her organs. There is no mixing of maternal and fetal blood in the placenta. In this section, you will learn about the circulation of blood through the fetus and placenta, and how the fetus is nourished and gets rid of its waste. The blood system in the placenta also limits what chemicals and infectious agents in the mother’s body can cross the placenta to endanger the life of the fetus.
As we mentioned in the previous section, the placenta starts to develop from the trophoblast, after the embryo implants in the uterus. It is fully developed within two months, and it continues growing until labour begins. The placenta weighs about 600 gm on average at delivery.
5.4.1 Fetal and maternal blood vessels
In order to understand how maternal and fetal blood is brought close together in the placenta, but does not mix, you must first learn some basic facts about blood and blood vessels. The cardiovascular system consists of the heart, the blood vessels (veins and arteries – see Box 5.2), and the blood that circulates around the body. It is the transport system that supplies oxygen and nutritive substances absorbed from the gastrointestinal system (gut) to all the cells, tissues and organs of the mother’s body and that of the growing fetus, enabling them to generate the energy they need to perform their functions. It also returns carbon dioxide, the waste product of respiration, to the lungs where it is breathed out. The chemical processes that go on in the body generate many waste products, which the blood transports to the kidneys and liver, where they are removed. Other functions of the cardiovascular system include the regulation of body temperature, and the circulation and delivery of hormones and other agents that regulate body functions.
Box 5.2 gives some key facts about the interaction of the maternal and fetal cardiovascular systems, and their relationship to the placental circulation.
Box 5.2 Key facts about the fetal, maternal and placental circulation
Oxygenated blood: Blood that carries enough oxygen and nutrients to the body’s cells, tissues and organs to enable them to function normally.
Deoxygenated blood: Blood that contains less oxygen and a higher proportion of dissolved wastes and carbon dioxide than is found in oxygenated blood.
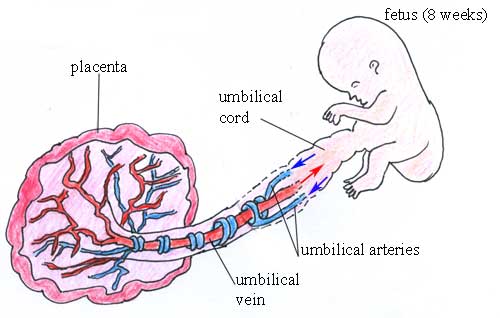
Umbilical arteries: Arteries usually carry oxygenated blood, but the two umbilical arteries (see Figure 5.4) collect deoxygenated blood from the body of the fetus and carry it to the placenta. The blood in the umbilical arteries is pumped to the placenta by the fetal heart.
Maternal veins: The mother’s veins collect deoxygenated blood from the placenta; as the blood passes through her liver and kidneys, dissolved wastes are removed — including those collected from the placenta by her endometrial veins. When the deoxygenated blood reaches the mother’s heart, it is pumped to her lungs to pick up more oxygen.
Maternal arteries: The mother’s arteries carry oxygenated blood around her body, pumped by her heart. Her endometrial arteries bring blood to her uterus and into the placenta, delivering oxygen from the mother’s lungs, and nutrients from her digestive system.
Umbilical vein: Veins usually carry deoxygenated blood, but the single umbilical vein (see Figure 5.4) carries oxygenated and nutrient-rich blood from the placenta and delivers it to the fetal heart, which pumps it around the body of the fetus.
5.4.2 The placental circulation
During fetal development, parts of the placenta project into the maternal endometrium. These small projections are called villi. They produce chemicals that digest and break open the walls of the mother’s arteries in the endometrium, so spaces in the placenta fill with oxygenated, nutrient-rich blood from the maternal endometrial arteries.
Villi (singular = villus) is pronounced ‘vill-eye’.
However, the pools of maternal blood in the placenta are not in direct contact with the fetal blood. The walls of the smallest fetal arteries and veins in the placenta — known as capillaries — remain intact (they are not digested). They are bathed on the outside by maternal blood, which is separated from the fetal blood inside the capillaries by the thickness of the vessel walls (Figure 5.5).
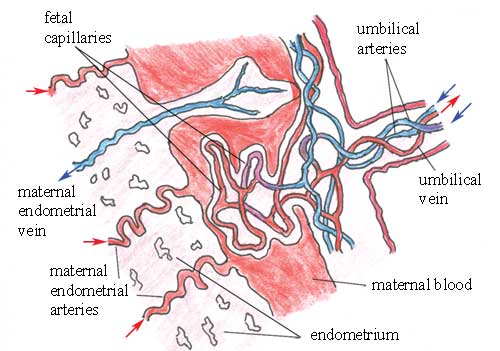
The fetal capillaries in the placenta are very close to the pool of maternal blood, which has a higher concentration of oxygen and dissolved nutrients than the fetal blood inside the fetal blood vessels.
Think back to your high school biology. What will happen to the oxygen and nutrients in the mother’s blood in this situation?
The oxygen and nutrients will move from the higher concentration in the mother’s blood, towards the lower concentration in the fetal blood. They will move through the walls of the fetal capillaries and into the fetal blood, by a process called diffusion. In this way, the fetal circulation is supplied with oxygen and nutrients.
How do you think dissolved waste in the fetal blood is removed as it passes through the placenta?
The concentration of dissolved waste in the fetal blood coming into the placenta is at a higher concentration than exists in the maternal blood bathing the fetal blood vessels. So the fetal waste diffuses through the walls of the fetal blood vessels and into the maternal blood, which carries the waste away to be removed by the mother’s liver and kidneys.
The placenta has a very large surface area, which facilitates the transport of substances in both directions by diffusion, as described above. Notice that the maternal blood never mixes with the fetal blood — they are always kept separated by the walls of the fetal blood vessels.
5.4.3 The placenta as a filter
One of the functions of the placenta is to act as a filter — allowing beneficial substances such as oxygen and nutrients to pass from the maternal circulation into the fetal circulation, but also trying to prevent harmful substances from making this journey. For example, the placenta allows the passage of some proteins and other bigger chemicals in the blood, including maternal antibodies — chemicals made by the mother to attack any infectious agents, such as bacteria that get into her body while she is pregnant. Allowing her antibodies to pass across the placenta and into the fetus is important in providing protection for the fetus, and later the newborn baby, against the same infectious agents.
However, the placenta cannot prevent the transfer of alcohol, other drugs and viruses to the fetus. These agents can cause birth defects, like discolouration of teeth, bone deformity and brain damage. Advising a pregnant woman to stop taking harmful drugs, and to reduce her exposure to harmful chemicals as much as possible, is very important. Your will learn more about this in Study Session 14 on health promotion issues in antenatal care.
5.4.4 Placental hormone synthesis
The placenta is an important hormone-secreting organ for much of the pregnancy. It secretes human chorionic gonadotropin (HCG), oestrogen and progesterone. The most commonly used pregnancy test detects HCG in the woman’s urine. The purpose of these hormones is to maintain the placenta, to keep it growing steadily as the fetus develops and gets bigger, and to prevent further ovulations and menstrual cycles, so the woman cannot become pregnant again until after the baby is born.
In the next study session, we consider a different interaction between the maternal and fetal anatomy — the bony structures of the mother’s pelvis and the fetal skull.
Summary of Study Session 5
In Study Session 5, you have learned that:
- Fertilisation involves the fusion of the male and female sex cells, the sperm and ovum, in the fallopian tubes.
- Sperm can survive in the female reproductive system for up to about 72 hours; the ovum lives for only 12 to 24 hours. For fertilisation to occur, sperm must be deposited in the vagina not more than three days before ovulation, or within 24 hours after ovulation.
- After fertilisation, cell division starts to form the developing embryo in stages, including the morula (solid ball of cells) and then the blastocyst (hollow ball of cells).
- Transportation of the embryo along the fallopian tube to the uterus takes about five to seven days.
- Implantation of the embryo takes place in the endometrium (lining) of the uterus. If it occurs in the fallopian tube, it is called an ectopic pregnancy, and this is very dangerous for the woman.
- The trophoblast region of the blastocyst penetrates the endometrium, and projections called villi secrete chemicals that dissolve maternal blood vessels. Maternal blood bathes the fetal blood vessels in the placenta, and nutrients, oxygen and dissolved waste is exchanged between mother and fetus.
- The maternal and fetal blood never mix in the placenta.
- The placenta functions as a transport site, a filter for beneficial and harmful substances, and a hormone-secreting organ.
Self-Assessment Questions (SAQs) for Study Session 5
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 5.1 (tests Learning Outcomes 5.1, 5.2 and 5.3)
Which of the following statements is false? In each case, say why it is incorrect.
A The energy for moving the sperm’s tail comes from the genetic material in its head.
B Contractions in the muscular walls of the uterus and fallopian tubes assist sperm to move rapidly towards the ovum.
C Implantation occurs when the blastocyst burrows into the endometrium and successfully establishes the early placenta.
D The umbilical vein transports deoxygenated blood from the fetus to the placenta.
E The placenta acts as a filter, preventing the transfer of all harmful substances from the mother to the fetal circulation.
Answer
A is false. The energy for moving the sperm’s tail comes from the mitochondria in the structure between the head and the tail.
B is true. Contractions in the muscular walls of the uterus and fallopian tubes assist sperm to move rapidly towards the ovum.
C is true. Implantation occurs when the blastocyst burrows into the endometrium and successfully establishes the early placenta.
D is false. The umbilical vein transports oxygenated blood from the placenta back to the fetus. The deoxygenated blood from the fetus is carried to the placenta by the two umbilical arteries.
E is false. The placenta cannot prevent the transfer of all harmful substances from the mother to the fetal circulation; for example, alcohol and other drugs and chemicals can diffuse through the placenta.
Read Case Study 5.1 and then answer the question that follows it.
Case Study 5.1 Advice for Mrs A after unprotected sex
Mrs A had unprotected sex (without a condom) 17 days after the first day of her last normal menstrual period. She visited your Health Post to ask you if there is a possibility that she could be pregnant.
SAQ 5.2 (tests Learning Outcome 5.2)
Explain the possibilities to Mrs A in language that she can understand.
Answer
Mrs A had unprotected sex on day 18 of her menstrual cycle. Ovulation occurs in most women around day 14, so she probably had sex within three to four days after ovulation. The ovum survives for only 12-24 hours unless it is fertilised, so if she ovulated as expected around day 14, then it is unlikely that the ovum was still alive when she had sex on day 18. Therefore, it is unlikely that she will be pregnant this time. But if her ovulation was later than expected, pregnancy is a possibility. Advise her about the risks of unprotected sex in terms of unwanted pregnancy and sexually transmitted infections.
Read Case Study 5.2 about Mrs P, and then answer the question that follows it.
Case Study 5.2 Mrs P asks why alcohol and khat can affect her fetus
Mrs P is a 38-year old pregnant woman who is addicted to alcohol and khat chewing. She attended an antenatal care health education session at your Health Post and listened to your explanation that ‘the maternal blood and fetal blood are not in direct contact’. Following this she asked you ‘Why are you telling me to stop taking alcohol and khat if my blood has no direct contact with my baby’s blood? If my blood has no direct contact, the alcohol and khat will not get into the baby’.
SAQ 5.3 (tests Learning Outcome 5.3)
What is your response? Explain it to her in language that she can understand.
Answer
You should explain to Mrs P that although her blood is not in direct contact with that of her baby, the two bloods are very close together in the placenta. Only the thickness of the baby’s blood vessel walls separates them. The walls are so thin that small substances like alcohol and khat can pass through them, from her blood to the baby’s blood. Tell her that this is also how good substances like oxygen and nutrients get into her baby from her own blood, so staying healthy and eating enough food is important for her baby’s development. If she stops taking alcohol and chewing khat, her baby will be much healthier. If she continues taking these harmful substances, the baby could be born with birth defects, or it could even die.