Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Tuesday, 10 February 2026, 11:34 AM
Antenatal Care Module: 15. Counselling Pregnant Women on Danger Symptoms
Study Session 15 Counselling Pregnant Women on Danger Symptoms
Introduction
This study session will provide you with the knowledge of how to counsel pregnant women on the common danger symptoms that some of them may develop in the course of their pregnancy. Effective counselling in language that the women in your community can understand will enable them to know when to get help quickly from you or from a health facility, if one of these danger symptoms develops.
You have already understood the different meaning of symptoms and signs in Study Session 8, and in Study Session 9 you learned about the common danger signs and symptoms during pregnancy. This study session will start by briefly explaining the general principles of counselling and the special features of counselling pregnant women. Then we summarise the common pregnancy-related or unrelated danger symptoms that pregnant women themselves can feel or notice in relation to the gestational age. Later in this session, we guide you about when and how to counsel pregnant women in relation to these danger symptoms, and we emphasise the importance of involving the husband/partner in this counselling.
Learning Outcomes for Study Session 15
After completing this session, you should be able to:
15.1 Define and use correctly all of the key words printed in bold. (SAQ 15.2)
15.2 Discuss the general principles of counselling and summarise the skills and attitudes of an effective counsellor. (SAQs 15.1, 15.3, 15.4 and 15.5)
15.3 Explain the special nature of counselling pregnant women. (SAQs 15.1 and 15.3)
15.4 Describe the common danger symptoms that can be felt or noticed by pregnant women, the gestational age at which each symptom is most likely to appear, and the appropriate actions that the woman should take. (SAQs 15.2 and 15.5)
15.5 Identify the appropriate timing of counselling on different types of danger symptoms, in relation to gestational age. (SAQ 15.3)
15.6 Explain the importance of husband/partner involvement in the counselling of pregnant women about danger symptoms. (SAQ 15.4)
15.1 General principles of counselling the pregnant woman
Counselling the pregnant woman is a process of two-way interpersonal communication in which you help her to know about possible problems that she may encounter during pregnancy, and make her own decisions about how to respond. When you create a two-way discussion with good understanding of each other, it not only helps the woman to know the possible problems that she may encounter and when to take appropriate action, but it also establishes a trusting relationship with you. Additionally, such two-way communication helps the woman to feel more comfortable and freely express her worries and needs to you.
Remember that the pregnant woman is also an expert on her own needs and situation. She has learnt informally many things about pregnancy (sometimes right and sometimes wrong). Therefore, never discourage her from expressing her beliefs and thoughts to you from the outset — you should develop tolerance for every woman’s values and beliefs, while you gently and sensitively try to dispel any important misconceptions she may have. Respect and tolerance for wrong beliefs doesn’t mean accepting that they cannot be changed. Sensitivity and tolerance are two of the most important qualities of an effective counsellor.
Box 15.1 summarises the skills and attitudes you need in order to develop good communication with any client, including pregnant women. The counselling process goes through the following stages: opening building relationships with pregnant women, exploring their issues, facilitating exchange of information (two-way) and closing the counselling process with gratification and the next appointment.
Box 15.1 Skills and attitudes for effective two-way communication
- Welcome the woman and ask her to sit near you and facing you.
- Smile and make good eye contact with her.
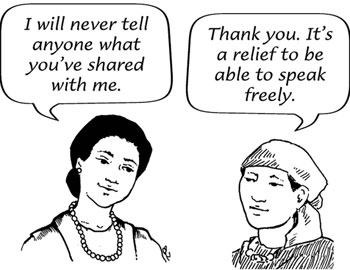
- Reassure her that you will always maintain her privacy and confidentiality (Figure 15.1).
- Without her permission, do not include a third person in the meeting.
- Use simple non-medical language and terminologies throughout that she can understand, and check frequently that she has really understood.
- Actively listen to her, using gestures and verbal communication to show her that you are paying attention to what she says.
- Encourage her to ask questions, express her needs and concerns, and seek clarification of any information that she does not understand.
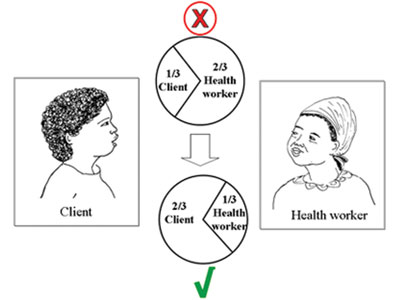
- Ideally, she should talk for about two-thirds of the time, and you talk for only one-third (see Figure 15.2). Research has shown that health professionals often talk too much, and don’t allow enough time for the client to express their own views and needs.
15.2 What is special about counselling pregnant women?
In the pregnant woman, the general purpose of counselling is to provide her with essential information for improving or maintaining her health and the health of her baby before and after birth. To be specific, the counselling will help the pregnant woman to stay healthy through advising her about health promotion issues such as nutrition (you learned about this in Study Session 14), and also to know the common symptoms of health risks that may affect her or her baby. In addition, counselling will be an entry point to the family, in particular to her husband/partner, so they also know the potential risks encountered during pregnancy and get prepared for them both psychologically and economically. Box 15.2 summarises the outcomes of successful counselling about danger symptoms during the antenatal period.

Box 15.2 Counselling about danger symptoms
Counselling has succeeded when the pregnant woman:
- Feels she got the help she wanted
- Understands the common danger symptoms
- Knows what to do and feels confident that she can come soon if she develops one of the danger symptoms
- Feels respected, listened to and appreciated
- Comes back when she needs your help (trusts you, see Figure 15.3).
15.3 What are the common danger symptoms during pregnancy?
The occurrence of the common danger symptoms that can be felt or noticed by the pregnant woman vary in their timing in relation to the gestational age.
What is meant by the first, second and third trimester of pregnancy?
Trimester means ‘three month period’. The first trimester is the first 3 months of the pregnancy (i.e. from conception to the 14th completed week of gestation, measured from the woman’s last normal menstrual period or LNMP); the second trimester is from 3-6 months (i.e. from 15 to 27 completed weeks); and the third trimester is the final 3 months of pregnancy (i.e. from 28 weeks to delivery at up to 42 weeks).
You have already learnt about the assessment of some pregnancy-related and medical problems by taking the woman’s history and doing a physical examination (recall Study Sessions 8 and 9). However, you can only detect health risks to the mother or to the baby during the routine antenatal checkups, so it is very important to help the mother detect any symptoms by herself and know when to come to you quickly.
First, you have to know very well the timing of occurrence of common pregnancy-related or other medical problems, taking the gestational age as the milestones (see Table 15.1). Secondly, you have to be selective not to overwhelm the pregnant mother with too much information at a time. Thirdly, remember that counselling is not a one-time business - you should be prepared to repeat the messages about danger symptoms at every visit and check that the woman has understood correctly.
You already know about some of the conditions listed in Table 15.1 (e.g. ectopic and molar pregnancy). Later in this Module, you will learn in detail about the other common causes of maternal and fetal mortality and morbidity during pregnancy: hyperemesis gravidarum was in Study Session 12; premature rupture of membranes (PROM) is in Study Session 17; malaria, anaemia and urinary tract infections are covered in Study Session 18; hypertensive disorders of pregnancy are in Study Session 19; and spontaneous and induced abortion and vaginal bleeding in early and late pregnancy are in Study Sessions 20 and 21 respectively.
On and off lower abdominal pain alone is very common in early pregnancy and is not a danger symptom on its own.
Symptoms the mother experiences (terms in italics are the most important) | She may have this medical condition |
|---|---|
| Conception to 20 weeks of pregnancy | |
| Persistent vomiting, weight loss | Hyperemesis gravidarum Characterised by persistent vomiting, weight loss of 5 kg and above, urine analysis shows ketones 2+ or more (You learnt about this in Study Session 12; how to do the urine analysis is in Study Session 19) |
| Vaginal bleeding (fresh), may include passage of clots and fleshy material, with crampy lower abdominal pain | Abortion (acute) All types of spontaneous abortions except missed abortion are acute ‘sudden’ events (You will learn about abortions in Study Session 20) |
| Pregnancy symptoms disappear, abdomen is not growing or is even decreasing in size, there may be minimal dark vaginal bleeding | Missed abortion When the fetus or fetal tissue is entirely in the uterus, but it has no signs of life and the cervix is completely closed |
| Vaginal bleeding (menstrual-like), lower abdominal pain, missed or irregular period | Ectopic pregnancy (covered in Study Sessions 5 and 12) |
| Vaginal bleeding (fresh), passage of tissues which look like an ice spoiled with blood (grape-like tissues), fast abdominal growth | Molar pregnancy (covered in Study Sessions 10 and 20) |
| 20 weeks to full term pregnancy | |
| Headache, burning epigastric pain (Figure 15.4), blurred vision, generalised body swelling (involving the back, abdominal wall, hands and face), decreased urine output | Hypertensive disorders of pregnancy (pre-eclampsia and eclampsia were introduced in Study Sessions 8 and 9; you will learn more in Study Session 19) 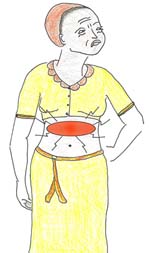 Figure 15.4 Burning epigastric pain is a danger symptom. |
| Vaginal bleeding in late pregnancy, even a minimal amount | Late abortion (20-27 weeks) or antepartum haemorrhage (28 weeks +) (You will learn more in Study Session 20) |
| Leakage of watery fluid from the vagina that wets her underwear significantly and may be extensive | Premature rupture of membranes (PROM) (You will learn about PROM in Study Session 17) |
| Progressively increasing pushing down pain in the lower abdomen before 9 months of gestation | Preterm labour (This is covered in the Module on Labour and Delivery Care) |
| No change in abdominal growth, fetal kick felt less than 10 times in 12 hours. (Any number of fetal kicks felt in one minute is counted as one kick) | Intrauterine fetal growth restriction (IUGR) (Briefly mentioned in Study Session 7) |
| Absent fetal kick for more than 6 hours | Intrauterine fetal death (IUFD) |
| At any time during pregnancy | |
| Fever, headache, chills, rigor, sweating, feels thirsty, generalised aching pain, lost appetite | Malaria, typhoid fever, typhus fever or relapsing fever (You will learn about these infections in the Module on Communicable Diseases)  Figure 15.5 Infection in this part of the kidney leads to danger symptoms. |
| Urination becomes painful, frequent, urgent and may be bloody or look like pus | Urinary tract infections (UTIs, cystitis or urethritis) (You will learn about UTIs in Study Session 18) |
| Pain in the sides (flanks), fever, vomiting, bloody urine, urgency and frequency in urination | Acute pyelonephritis (Figure 15.5 shows the specific area in the kidney where this infection can occur) |
| Yellowish discolouration of the eyes, loss of appetite, hate spicy food smell, feels exhausted, nausea and vomiting | Liver disease |
| Thirsty, drinks excessive amounts of water, urinates a lot, feels hungry, weight loss | Diabetes mellitus |
| Persistent cough | Lung and heart disease |
Table 15.1 is a detailed summary for you to study as a healthcare provider. It would not be appropriate or useful to show it to pregnant women during antenatal visits.
Can you suggest why not?
The table uses medical language that the woman is unlikely to understand (unless she is also a health worker), and it may overwhelm her with too much information all at once and make her anxious to see so many potential risks to herself and her baby.
Table 15.2 is a simplified summary in two parts, which can be shared with pregnant women at the appropriate stage of gestation. Women in the basic component of the focused antenatal care (FANC) programme, described in Study Session 13, should be seen for the first antenatal visit before 16 weeks of gestation if possible, and for the second visit at 20-24 weeks. Make sure every woman knows the common danger symptoms that are more likely to occur at each stage.
| In all visits before 20 weeks | In all visits after 20 weeks |
|---|---|
Persistent vomiting Vaginal bleeding No change in abdominal growth Fever Vomiting | Headache Burning epigastric pain (see Figure 15.4) Blurred vision Vaginal bleeding Leakage of fluid No change in abdominal growth Persistent vomiting |
15.4 Telling pregnant women about the danger symptoms
You should realise that pregnant women have many responsibilities at home and usually also in the fields, and they may already be overwhelmed by too much information about the current pregnancy. Table 15.2 presents what the mother primarily needs to know, but you shouldn’t tell her everything all at the same time. Counselling the pregnant woman in relation to the stages of pregnancy is a good strategy from the perspective of the pregnant woman’s understanding and using your time as efficiently as possible. In other words, you need to discuss the common danger symptoms with her, taking into account the stage of pregnancy. For instance, a pregnant woman coming for antenatal care before 20 weeks of gestation should be counselled about the danger symptoms of miscarriage, which are usually manifested by vaginal bleeding. She should also be aware of danger symptoms of common medical disorders that can occur any time during pregnancy - in the same way that they could occur to anyone in the rest of the population.
Most pregnancy-related serious problems occur in the third trimester. Therefore, it is a good opportunity to counsel the mother about them during the second trimester, to let her prepare ahead of time. If you have them, using printed instructions, diagrams, photos or pictures, which improve the pregnant woman’s understanding and her ability to remember the key points. It is also a good approach to remind her about what was discussed at earlier antenatal visits (see Box 15.3).
Box 15.3 Following up on previous counselling messages
In subsequent antenatal visits, helping the woman to go over what was discussed before will help you to:
- Discover how much she understood the issue already
- Discover how much she can recall correctly
- Identify her acceptance and readiness to act on the knowledge
- Identify areas she has wrongly understood.
It will also help her to express her concerns and doubts, so that you can:
- Discuss any issues that were not clear or not accepted
- Plan together what to do next, involving her husband/partner.
15.5 Advantages of husband/partner involvement in antenatal counselling
The majority of pregnancy-related problems are unpredictable and late phenomena. On the other hand, public awareness of pregnancy-related maternal and fetal health risks is very minimal. So far in Ethiopia, the husband or male partner is usually more influential, economically empowered and socially accepted than the woman. Counselling as many pregnant women as possible is one way of accessing the public by involving the husband, who can act as the second agent on dissemination of potential risks of pregnancy to the majority (the public).
Therefore, involving the husband/partner in antenatal visits has many advantages (Box 15.4).

Box 15.4 Involving the husband/partner in antenatal visits
- Helps the partner/husband to become aware of the danger symptoms the woman may encounter during the pregnancy.
- Will make him more caring and more concerned.
- Helps him to take action (early reporting) when danger symptoms appear.
- Alerts him to save money for possible emergencies, e.g. transport to the health facility.
- Alerts the family to decide on their preferred place of delivery.
- Helps the family get prepared for caring for the mother and her baby after the birth.
- Is a further entry point to increase general public awareness of the potential risks during pregnancy.
15.6 Checklist after each antenatal counselling session
Finally, we conclude this study session with a checklist that you can use to evaluate your own counselling skills and attitudes (Table 15.3). It has been adapted for use in counselling pregnant women, but it incorporates the general principles of counselling that you can apply to any client in your health care.
| Greet | Did you: |
|---|---|
Welcome each pregnant woman on arrival? Discuss in a comfortable and private place? Assure the pregnant woman of confidentiality? Express caring and acceptance by words and gestures throughout the meeting? Explain what to expect? | |
| Ask | Did you: |
Ask the pregnant woman’s reason for the visit? Encourage the pregnant woman to do two-thirds of the talking? Ask mostly ‘open’ questions? Pay attention to both what the client said and how it was said? Put yourself in the woman’s shoes — expressing understanding of what she said without criticism or judgment? Ask about the pregnant woman’s feelings? Ask about her preferences? | |
| Tell | Did you |
Start the discussion focusing on the pregnant woman’s preference(s)? Discuss the danger symptoms of pregnancy in relation to the gestational age? Give information about danger symptoms of pregnancy to help her make her own decisions? Avoid ‘information overload’? Use words familiar to the client? Discuss the advantages of early reporting if she encountered danger symptoms during pregnancy? | |
| Help | Did you: |
Let the pregnant women know that the decision is hers? Help the pregnant women be able to realise common danger symptoms? Help her think over the consequences for her own or her baby’s life? Advise the pregnant women without controlling and frustrating? Let the pregnant women decide? Make sure the pregnant women’s choices are based on accurate understanding? List any medical, social, cultural or religious reasons for making a different decision – probably different from what you might like to achieve? | |
| Explain | Did you: |
Provide what the client wants, if there is no medical reason not to? Explain when the woman should come to you if one of the danger symptoms appeared? Help her to explain in her own words how much she understands each of the danger symptoms of pregnancy? Explain using printed instructions, pictures and diagrams? | |
| Return | Did you: |
Plan when the next visit should be? Discuss with the pregnant woman if she can come back with her husband or partner? Assure the pregnant woman that she should come back at any time, for any reason? Assure her to come back soon, even if she missed the day of her scheduled appointment for some reason beyond her control? Assure her that it is her full right to go to any other health facility at any time? Thank the pregnant woman for attending for antenatal care? |
Summary of Study Session 15
In Study Session 15 you learned that:
- Counselling is a two-way confidential communication process that helps pregnant women to examine their personal issues, make decisions, and make plans for taking action if they develop danger symptoms.
- Basic skills in counselling include the use of active listening, encouraging the pregnant woman to talk, to ask questions freely, and focusing on relevant issues in relation to danger symptoms and gestational age.
- Every pregnant woman has the right to decide what happens to her pregnancy.
- All information that the pregnant woman provides during her visit should be kept confidential.
- Common errors in counselling include interrupting the woman when she is talking, looking away frequently, criticising her cultural and religious values, finishing off her sentences and judging her.
- The counselling process goes through the following stages: opening and building relationships, exploring the issues, facilitating change, and closing.
- The pregnant woman should be counselled to come to you at once if she develops one or more of the following danger symptoms:
- Usually in the first half of pregnancy: persistent vomiting, weight loss, vaginal bleeding and no change in abdominal growth.
- Usually in the second half of pregnancy: headache, blurred vision, epigastric burning pain, vaginal bleeding, leakage of fluid from the vagina, no change in abdominal growth, decreased or absent fetal kick.
- Any time during pregnancy: fever, vomiting, flank pain, yellowish discoloration of eyes or persistent cough.
- Involving the husband or partner in the antenatal care visits makes care of the pregnant woman a family concern and responsibility, and also helps them to be alert to danger symptoms that need urgent action.
Self-Assessment Questions for Study Session 15
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 15.1 (tests Learning Outcomes 15.1 and 15.2)
For each of the following statements, say whether it is true or false. Explain what is incorrect about any statement that you judge to be false.
A Saying welcome, showing a smiling face, letting her express her concerns and doubts, helps the mother feel comfortable and develop confidence in you.
B You have to tell her that unless she comes on the day of her scheduled appointment, you will not see her at any other time.
C You should not allow her to ask questions till you finish telling her what she needs to know.
D You can counsel one woman who is sitting with you while you are conducting a physical exam of another one.
E If she tells you that her two daughters were circumcised on the day she gave birth at home, tell her harshly that she shouldn’t do it again, and if she plans to do the same thing if this baby is a girl, she should not come back for any other visits.
F Counselling a pregnant woman on danger symptoms is essential in every visit.
Answer
A is true. Welcoming the mother, smiling and letting her express her concerns and doubts, helps her to feel comfortable and develops confidence in you.
B is false. It is not an easy task always to come on the day of appointment for the majority of rural Ethiopian pregnant women, who typically have many personal and social responsibilities at home. It is their right to come earlier or later than the appointed date, or even not to come at all. It is the duty and responsibility of any health professional to say welcome with open hands at whatever time and date women come for their antenatal check-up.
C is false. The health service is primarily the client’s/patient’s business. The duty of the health professionals is to deliver a service which makes the client comfortable and satisfied. With that understanding, you have to be prepared to receive questions and do the best to encourage women to raise any questions which are not clear for them.
D is false. By its principle, counselling is discussing personal issues which the client may not like to be shared with other persons outside the family. Therefore, even when you are in a hurry, it is not advisable to counsel one woman while you are examining another. In such an environment, the one to be counselled may not freely share her feelings and concerns with you.
E is false. You cannot encourage behavioural change in adults by criticising, frustrating, demoralising and openly discouraging them. This woman will not feel respected by you and she may not return for further antenatal care. To make a positive change in unhealthy behaviour, the best method with adults is open discussion, letting them know the risks/disadvantages and giving them a chance to evaluate the options for themselves and make their own decision.
F is true. During every antenatal care visit, pregnant women should be counselled on the danger symptoms of pregnancy, so they can take swift action if an emergency arises.
SAQ 15.2 (tests Learning Outcome 15.3)
Based on what you have learned from Table 15.1, match each of the danger symptoms with the appropriate medical condition.
Two lists follow, match one item from the first with one item from the second. Each item can only be matched once. There are 6 items in each list.
Leakage of fluid from the vagina
Vaginal bleeding
Fever
Abdominal size decreasing
Flank pain
Persistent headache
Match each of the previous list items with an item from the following list:
a.Antepartum haemorrhage
b.Hypertension
c.Malaria
d.PROM
e.Acute pyelonephritis
f.Missed abortion
- 1 = d,
- 2 = a,
- 3 = c,
- 4 = f,
- 5 = e,
- 6 = b
SAQ 15.3 (tests Learning Outcome 15.4)
For each of the following statements, say whether it is true or false. Explain what is incorrect about any statement that you judge to be false.
A. The counsellor should tell the pregnant woman about all the danger symptoms of pregnancy during her first focused antenatal visit before 16 weeks of gestation.
B. Encouraging the pregnant woman to repeat what has been discussed during counselling will increase her memory (retention capacity) of the key points.
Answer
A is false. The area of counselling that pregnant women need should be appropriate to their stage of pregnancy, because:
- Different pregnancy-related complications occur at different stages of pregnancy.
- It is not easy for clients to understand and retain a lot of information, particularly if it is not relevant to them at that time.
- Addressing all the danger symptoms during a single visit will take a lot of your time.
- So much potentially worrying information about dangers may overwhelm the clients, and prevent them from raising their own questions and asking for clarification.
B is true. Repeating what has been discussed/said will help:
- The pregnant woman to remember what she has heard.
- The health service provider to check the woman’s level of understanding.
SAQ 15.4 (tests Learning Outcome 15.5)
List some of the advantages of involving the husband/partner in antenatal counselling on danger symptoms.
Answer
- Counselling the husband/partner on the danger symptoms during antenatal visits means that he can also look out for them and get help more quickly in an emergency.
- Involving husbands/partners is one way of informing the public more widely about the potential risks to women and babies during a pregnancy.
- If the husband/partner knows the possible health risks of pregnancy, he may be more caring and more concerned about looking after his wife.
- He is more likely to agree to take his pregnant wife to a health service provider if danger symptoms arise.
- Counselling the husband/partner enables him to get prepared both psychologically and financially for dealing with a possible pregnancy-related emergency.
First read Case Study 15.1 carefully and then answer the questions that follow it.
Case study 15.1 Mrs H’s story
Mrs H is a 25-year-old woman in her second pregnancy, who came to see her Health Extension Practitioner (HEP) for the first time when she was 34 weeks pregnant. The HEP asked where she gave birth previously. Her blood pressure and weight was measured and her general health seemed good; her abdomen was examined, and the pregnancy seemed to be progressing normally. Lastly, she was told to come back after 3 weeks.
Two weeks later, she developed excess leakage of watery fluid from her vagina. She informed her neighbours and they told her not worry about it. Since it continued flowing, on the third day after the leakage began, she went back to the HEP and got the same advice she got at home. On the fifth day, she developed a high fever (temperature 39oC) and an offensive smelling vaginal discharge.
SAQ 15.5 (tests Learning Outcomes 15.1 to 15.5)
- a.What is wrong with the antenatal visit at 34 weeks’ gestation from the perspective of counselling the pregnant woman effectively?
- b.Why did Mrs H leak watery fluid from her vagina?
- c.Why did she wait three days to report to the HEP after the leakage began?
- d.What should have been done by the HEP when Mrs H came with leakage of fluid from her vagina?
- e.Why did Mrs H develop a high fever and offensive smelling vaginal discharge?
Answer
- a.Mrs H was not counselled on the danger symptoms of pregnancy at 34 weeks’ gestation. When she was worried about her symptoms, she requested advice from her neighbours. They thought (incorrectly) that the leakage of watery fluid from her vagina at 36 weeks was normal, instead of a serious pregnancy-related problem.
- b.The watery fluid leaked because of the premature rupture of fetal membranes that function as a sac to hold the fetus and the amniotic fluid inside. So, it was the amniotic fluid which was coming out through the broken membranes.
- c.She waited days before seeking help because she did not know fluid leakage is a danger sign of PROM (premature rupture of membranes) and her neighbours assured her that it was not a problem.
- d.The HEP should have referred her to the nearest health centre or hospital for evaluation and treatment.
- e.Mrs H developed a high fever and offensive smelling vaginal discharge because infection was able to rise up through the vagina into the uterus after the fetal membranes ruptured.