Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 5 February 2026, 7:36 AM
Antenatal Care Module: 21. Late Pregnancy Bleeding
Study Session 21 Late Pregnancy Bleeding
Introduction
Bleeding after 28 weeks of gestation is considered to be late pregnancy bleeding. You learned about early pregnancy bleeding before 28 weeks in Study Session 20. Late pregnancy bleeding is also referred to as antepartum haemorrhage (APH) by doctors and midwives. It is an important cause of maternal and fetal death and needs the attention of a highly skilled heathcare provider at the earliest time possible in order to save the life of the woman and her unborn baby.
‘Antepartum’ is Latin for ‘before birth’; ‘haemorrhage’ is pronounced ‘hemm-orr-edge’ and means severe loss of blood.

As the first contact provider for pregnant women in your community, you have to work with them on birth preparedness and making a complication readiness plan to address such eventualities as severe bleeding in pregnancy. You must provide obstetric first aid and then make sure that a woman with late pregnancy bleeding can reach a health facility where she can get urgent help. A District Hospital or Health Centre with the ability to perform obstetric operations can save her life.
Learning Outcomes for Study Session 21
When you have studied this session, you should be able to:
21.1 Define and correctly use all of the keywords printed in bold. (SAQs 21.2 and 21.3)
21.2 Describe the warning signs and the common causes of late pregnancy bleeding. (SAQs 21.1, 21.2 and 21.3)
21.3 Provide obstetric first aid and know when to make an urgent referral of a woman with late pregnancy bleeding. (SAQs 21.1 and 21.2)
21.1 What causes late pregnancy bleeding?
The most common causes of late pregnancy bleeding, or ante-partum haemorrhage (APH), are due to bleeding from the placenta, but there are other less common causes arising in the uterus or other parts of the reproductive tract. First, we will list the causes briefly, and then describe placental abruption, placenta previa and ruptured uterus in detail, because these are conditions that require your immediate life-saving intervention.
- Placental abruption: this condition occurs if the placenta pulls away prematurely (too soon) from its normal attachment site in the top two-thirds of the uterus.
- Placenta previa: this condition is when the placenta has attached too low down in the uterus, very close to, or even covering, the cervix.
- Ruptured uterus: this can occur during a prolonged or obstructed labour when the uterus, after a long effort to expel the fetus, gives way and tears or bursts.
- Ruptured varicose vein in the genital area: this can occur if a vein becomes twisted and dilated. As a result, it can easily be traumatised and bleed, usually during labour and delivery.
- Heavy show: the mucus mixed with bloody fluid that comes from the birth canal at the start of labour is called the show; sometimes, when this mucus plug detaches it may be followed by brisk and heavy bleeding called a heavy show, which often stops on its own without any intervention. But she should always be referred.
21.2 Placental abruption
Placental abruption refers to the premature separation of the whole or part of a placenta which is implanted in the upper two-thirds of the uterus. Normally the placenta only separates from the uterus after the delivery of the fetus, in the third stage of labour (you will learn all about this in the module on Labour and Delivery Care). The mother and the baby may die if the place where the placenta pulled away from the wall of the uterus starts to bleed a lot.
Why is it likely that placental abruption will result in a lot of bleeding, and why does this pose a serious risk to the mother and the fetus? (Think back to what you learned about the structure of the placenta in Study Session 5, or look again at Figure 5.5 in Antenatal Care, Part 1.)
the mother’s blood flows into large spaces in the placenta which lie close to the fetal blood vessels (Figure 5.5). If the placenta tears away from the wall of the uterus, the mother’s blood will flow out into the cavity of the uterus and she could die from the loss of blood. The supply of oxygen and nutrients from her blood to the fetus will be reduced, so it may die or be severely brain damaged.
Most of the bleeding from the place where the placenta has pulled away from the wall of the uterus may escape through the cervix and flow out of the vagina. This blood is usually dark in colour because it doesn’t contain much oxygen. This is an important warning sign!
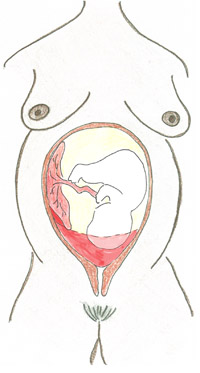
However, in some cases, all the blood from the detachment site may stay inside the uterus cavity, which begins to fill up with blood (Figure 21.1). You will not see external bleeding, as very little of the blood escapes through the vagina. However, the woman will show the typical signs of severe internal bleeding known as haemorrhagic shock, which we already described briefly in Study Session 20 on early pregnancy bleeding. We repeat the information below (Section 21.2.1) because there is even more risk of it happening when a woman bleeds late in the pregnancy.
Other signs of placental abruption include:
- If the mother is already in labour, notice if she has pain between contractions, which may get worse and worse as time passes
- Her abdomen is hard, sore and tender to the touch
- The baby’s heartbeat can be very fast (faster than 180 beats a minute), or very slow (slower than 100 beats a minute), or if you cannot hear a fetal heartbeat the baby could be dead
- The baby moves less or not at all.
21.2.1 Haemorrhagic shock
![]() All of the conditions resulting from placental abruption require you to take immediate emergency action: see Section 21.5.
All of the conditions resulting from placental abruption require you to take immediate emergency action: see Section 21.5.
Placental abruption with external or internal bleeding may lead to haemorrhagic shock, in which blood is lost in such large amounts that the blood remaining in the woman’s blood vessels is not enough to deliver the nutrients and oxygen required by her body cells.
What are the signs and symptoms of haemorrhagic shock? (Think back to Box 20.3 in the previous study session.)
A woman in shock will be pale and sweating, with a fast but feeble pulse (above 100 beats per minute), fast respiration, low or falling blood pressure (the diastolic pressure — the bottom number — is no more than 60 mmHg and sometimes far less); she complains of dizziness; she seems confused and may even lose consciousness.
You should look for signs such as pallor: her fingernails, the palms of her hands and the inside of her eyelids will turn whiter as she loses blood. She may tell you she feels weak or be unable to lift her head. She appears restless, possibly asking for water to drink, and she seems confused. Confusion happens because her brain is being starved of oxygen. Common consequences of haemorrhagic shock include failure of the kidneys or the heart.
21.2.2 Acute renal failure
As a result of haemorrhagic shock and the reduced amount of blood flowing to the kidneys, they may stop functioning. As a result, the woman produces very little urine, so toxic material which should have been cleared from her blood by her kidneys and expelled in her urine will build up in her blood. The accumulation of toxic chemicals in her blood rapidly causes her to become severely ill and death follows unless the condition is reversed. This condition is called acute renal failure (‘acute’ means it develops quickly into a life-threatening condition; ‘renal’ is a medical term referring to anything to do with the kidneys).
21.2.3 Heart failure
If the woman is haemorrhaging, her heart will beat very fast as it tries to pump enough blood to vital body parts like her brain. If the blood loss is severe, her heart may not be able to beat fast enough to compensate for the falling blood volume and the women will develop heart failure. This condition is where the heart is unable to pump enough blood to the tissues and as a result death may occur.
21.3 Placenta previa
The other common cause for late bleeding is placenta previa. In this situation the placenta is attached very close to the cervix, or is even covering it (Figure 21.2). As the cervix dilates the edge of the placenta may detach and it starts bleeding. A woman with this condition generally has clear, bright red blood coming from her vagina. The amount may be less than with placental abruption, but in some cases it can be severe and life threatening. The bleeding is often painless, so the woman may not have noticed it happening for a while, for example during the night when she was in bed. The bleeding can be set off by sexual intercourse and it may be recurrent (stopping and starting again).
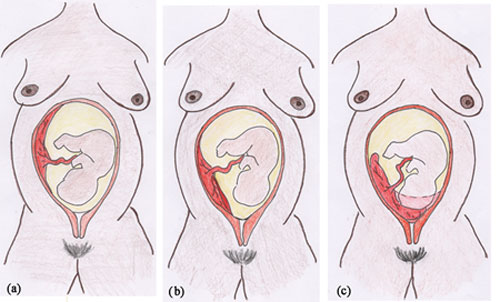
In a woman with late pregnancy bleeding due to placenta previa, the uterus often feels soft when you palpate her abdomen, in contrast to the hard feeling of the uterus when bleeding is due to placental abruption.
The fetal head is generally not in the lower part of the uterus, which feels empty. This abnormal presentation may be a sign of placenta previa. Usually the fetal condition is normal, so you can detect a fetal heart beat when you listen with a fetoscope, and the mother reports the fetus is moving and kicking normally — but this is not always the case.
The diagnosis of placenta previa can only be confirmed by examining the woman with an ultrasound machine that can reveal the position of the placenta, or by vaginal examination in an operating theatre. Therefore you should refer her to a health facility with the necessary equipment to make a diagnosis.
![]() Women with a suspected placenta previa should be referred to a District Hospital or Health Centre with an ultrasound machine or operating theatre.
Women with a suspected placenta previa should be referred to a District Hospital or Health Centre with an ultrasound machine or operating theatre.
Never do a vaginal examination yourself if a woman is bleeding in late pregnancy. This will worsen the situation and increase the risk to her and the fetus.
21.4 Ruptured uterus
Bleeding from a ruptured uterus may occur from the vagina so you can see the blood flowing out, or the uterus may bleed into the woman’s abdomen where the blood won’t be visible to you. If a woman who has been a long time in labour develops abdominal pain that is constant and gets worse with movement, or if, the uterus stops its contraction in the effort of expulsing the fetus, or she develops vaginal bleeding with associated state of shock, it is likely that the uterus has ruptured. If the uterus stops contracting, the abdomen will become soft and the fetal parts can be felt easily when you do an abdominal examination. If the baby has died the fetal heartbeat will not be evident when you listen with a fetoscope.
You will learn much more detail about the condition of the ruptured uterus in the next module in this curriculum, on Labour and Delivery Care. If you encounter a woman with the signs of a ruptured uterus you should take the emergency actions described below.
21.5 What to do for a woman with late pregnancy bleeding
If you detect late pregnancy bleeding and you suspect placental abruption, placenta previa, a ruptured uterus or bleeding from any other cause, take the following steps:
- Never perform a vaginal examination
- Make a rapid evaluation of the general condition of the woman, including vital signs: pulse, blood pressure, respiration and temperature; check her for pallor, weakness, dizziness and confusion.
- If you suspect shock, begin treatment immediately by starting a rapid intravenous (IV) infusion with Normal Saline or Ringer’s Lactate solution. (You will learn the theory of how to do this in Study Session 22 and develop this competency in your practical skills training.)
- Even if signs of shock are not present, keep shock in mind as you evaluate the woman further because her status may worsen rapidly. If shock develops, take the actions described above.
- Urgently mobilise all available people who can help, inform them how serious the situation is and put into action the complication readiness plan you developed with the woman and as part of focused antenatal care (Study Session 15 of this module). For example, get the village people to assist with transporting her quickly to the higher health facility; make sure that healthy people go with her who can donate blood if she requires a blood transfusion.

Remember that the initial bleeding could be heavy and life-threatening and the woman may arrive at your Health Post carried by relatives. In such a situation, after you do a quick assessment of the condition of the patient, put up the IV line, organise transport and send the woman to the nearest higher health facility as soon as possible.
What is the safest position in which to transport the woman? (Think back to Figure 20.3 in the previous study session.)
Her head should be lying flat — don’t put a pillow under her head. Raise her knees and support her legs with pillows or rolled blankets, so her feet are higher than her head.
 In the case of late pregnancy bleeding, even if the bleeding stops on its own before labour begins, the woman should always be referred and preferably deliver her baby in a higher health facility.
In the case of late pregnancy bleeding, even if the bleeding stops on its own before labour begins, the woman should always be referred and preferably deliver her baby in a higher health facility.
Ideally, you should accompany her to maintain the IV infusion and keep the bag of IV fluid held above her. If you cannot go with her, explain the importance to whoever accompanies her of keeping the woman and the fluid bag in the suggested positions; also tell them how to close the IV tubing when the bag of fluid has completely drained. Remember to send a referral note with the woman.
In the final study session in this Module, we teach you the theory of how to set up an intravenous infusion, and also how to insert a urinary catheter in a woman who is unable to urinate due to complications of pregnancy or labour.
Summary of Study Session 21
In Study Session 21 you have learned that:
- Late pregnancy bleeding (ante-partum haemorrhage) can cause maternal and fetal death, and should be treated as a potentially life-threatening emergency.
- The most common causes of life-threatening late pregnancy bleeding are placental abruption and placenta previa, or more rarely it can result from a ruptured uterus.
- Less serious bleeding can arise from a varicose vein in the genital area, or blood resulting from a heavy show, which usually stops on its own.
- Placental abruption can present with both concealed (internal) and revealed (externally visible) bleeding from the vagina; the blood is usually dark and the woman may report abdominal pain.
- Placenta previa often presents with painless, bright red bleeding and can be associated with abnormal presentation of the fetus. Usually (but not always) fetal condition is normal.
- Never do a vaginal examination in women with late pregnancy bleeding as this may precipitate severe bleeding.
- Initial assessment of the woman’s vital signs and initiation of IV fluid therapy are the critical first steps in managing haemorrhagic shock in women with severe late pregnancy bleeding.
- After putting up an IV infusion, transfer the patient immediately to a District Hospital or higher health facility with an operating theatre, as most cases require surgical intervention.
Self-Assessment Questions for Study Session 21
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 21.1 (tests Learning Outcomes 21.2 and 21.3)
Relatives call you to see a woman who is bleeding from the vagina at the 8th month of gestation.
- a.What will you do as the initial assessment?
- b.Will you initiate emergency treatment for this woman and refer her to the nearest higher health facility? Explain why, or why not.
- c.What will you tell the relatives to do?
Answer
- a.The initial assessment would be a rapid evaluation of the general condition of the woman, including her vital signs: pulse, blood pressure, respiration and temperature; check her for pallor, weakness, dizziness and confusion.
- b.Emergency treatment should begin immediately with rapid intravenous (IV) infusion with Normal Saline or Ringer’s Lactate solution. This may save her life by replacing the fluids and salts lost through the haemorrhage, so her blood pressure does not drop dangerously low.
- c.The relatives should be told to organise transport for the woman to the nearest higher level health facility.
SAQ 21.2 (tests Learning Outcomes 21.1, 21.2 and 21.3)
Which of the following statements is false? In each case, say why it is incorrect.
A You can do a vaginal examination for a pregnant women who comes to you with vaginal bleeding at gestational age of 37 weeks.
B Premature separation of a normally implanted placenta always results in external bleeding.
C Placenta previa is when the placenta is attached close to or covering the cervix.
D You may not need to refer women who present with persistent or recurrent bleeding in late pregnancy if the bleeding stops spontaneously.
Answer
A is false. You should never do a vaginal examination on a woman with late pregnancy bleeding (i.e. after 28 weeks of gestation).
B is false. Premature separation of a normally implanted placenta may result in external bleeding, but it may also cause internal bleeding.
C is true. Placenta previa is when the placenta is attached close to or covering the cervix.
D is false. You should always refer women with persistent or recurrent bleeding in late pregnancy, even if the bleeding stops spontaneously.
Read Case Study 21.1 and then answer the questions that follow it.
Case Study 21.1 Mrs X is brought to the Health Post
Mrs X is brought to your Health Post carried by her relatives on a locally made wooden bed. You are told she is 9 months pregnant. She had severe abdominal pain, which was followed by vaginal bleeding. When you examine her you see her clothes are soaked in blood. She is restless and asking for water. Her pulse is 120 beats per minute and her blood pressure is 80/50 mmHg.
SAQ 21.3 (tests Learning Outcomes 21.1 and 21.2)
- a.What are the possible causes of bleeding in this case? Explain your answer.
- b.Is Mrs X in a state of shock? Justify your diagnosis.
Answer
- a.The possible causes of bleeding in the case of Mrs X are:
- Placental abruption
- Placenta previa
- Ruptured uterus
- Ruptured varicose vein.
- b.Mrs X is in a state of shock: she is restless and thirsty, her pulse is very fast (120 beats/minute) and her blood pressure is dangerously low (80/50 mmHg).