Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Wednesday, 21 January 2026, 10:12 PM
Your healthcare practice
Introduction
Welcome to Section 3 of the Introducing practical healthcare course, where you will explore a number of concepts regarding healthcare practice. When completed you will have the opportunity to obtain a ‘Your healthcare practice’ badge. This section will take approximately 3 hours to complete.
Here you will consider the privacy and dignity of patients, with a particular focus on how to provide intimate care for those who are ill (for example, the bedridden or in hospital). You will learn about the importance of fluids and nutrition, and a number of important factors to consider when trying to maintain a healthy diet for the patient.
Another important part of this section is about how to maintain health and safety within your workplace, and the need for infection prevention and control, covering hand hygiene, safe disposal of waste, safe management of laundry, and Personal Protective Equipment (PPE) such as masks and goggles to protect from injury and infection. Lastly, this section of the course will aim to raise your awareness of mental health, dementia and learning disabilities, by providing definitions and specific types to look out for so that you can respond in the most appropriate way.
Learning outcomes
By completing this section and the associated quiz, you will be able to:
explain why it is important to respect privacy and dignity in personalised care
demonstrate awareness of health and safety regulations at work.
1 Privacy and dignity
In order to deliver good healthcare and support, you must practise two important values: privacy, which means giving someone space where and when they need it, and dignity, which means focusing on the value of every individual. To achieve this you must respect their views, choices and decisions; enable them to be as independent as possible; not make assumptions about how they want to be treated; always work with care and compassion; and communicate as directly as you can with them.
In the next audio clip you can clearly hear how much Gail (a healthcare assistant) loves her job, and how she always works with utmost compassion for her patients.
Transcript: A healthcare assistant who loves her job
You should always provide personalised care and support that puts an individual at the centre of their care. When you first meet a new patient you should tell them your name and what your role is, and ask them what they want you to call them. Becoming ill usually has an adverse effect on people, whatever their age or background. Patients are likely to be worried about the unknown, so remember that your patient may well be experiencing fear of what lies ahead, and applying these values will go some way to reassuring them and enable them to be as independent as possible (Skills for Care, 2015, p. 2).
Good personal hygiene is an important part of maintaining dignity. Providing intimate care can be a particular challenge for newer healthcare assistants. Bodily functions like washing, dressing and toileting are normally kept very private, and might seem difficult because of cultural or personal background, gender issues and social awkwardness. Most inpatients expect to maintain their normal standards of hygiene – and this should be recorded on their care plan. You should always enable the patients to do as much as possible for themselves, but they may need help to wash and you should be aware that they may be feeling embarrassed or humiliated by being needy in this way. Whether using the bathroom or washing a patient in bed, you will need to ensure the water temperature and depth of the bath water are appropriate, and whilst making sure the person’s dignity is protected, end up with them being clean and refreshed. Careful attention to cleanliness of the mouth and feet is also important, by giving attention to these details it shows a patient that you are really doing your best to make them as comfortable as you can.
Activity 1
2 Fluids and nutrition
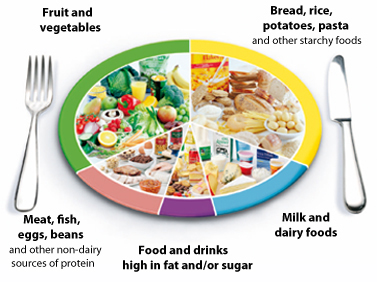
According to the UK Food Standards Agency (FSA), a normal balanced diet should include about one-third fruit and vegetables, and one-third bread, rice, potatoes, pasta and other starchy foods (carbohydrates). The remaining third of the diet should be made up of about equal quantities of meat, fish, eggs and beans (sources of protein) and of milk and dairy foods, with ideally only a small amount of foods and drinks that are high in fat and/or sugar. This is illustrated in the FSA’s ῾eatwell plate᾿ (Brown, 2010).
People who are ill particularly need fluids and nutrition to help them get better, and as a healthcare assistant maintaining appropriate levels of these in accordance with patients’ care plans will form a major part of your day-to-day work. Caring for patients who find eating and drinking difficult can however pose a big challenge for healthcare staff, and recent reports have shown evidence of severe problems in this area.
Nutrition is more than calories; our diets must be balanced and contain a range of vital nutrients which are important to remember. Some medical conditions will require a diet which is high or low in some of them. These nutrients include:
- carbohydrates for energy
- protein for body repair
- fibre to help our digestion and remove waste products
- minerals for our bones, teeth, blood and nerves;
- vitamins to regulate many of the body’s systems and functions (OpenLearn, 2011).
It might seem that patients in hospital would need less food than normal, because they’re less active, and this is true for some but not all. Many people are underweight when they come for treatment or admitted to hospital and need building up, whereas other people with excess weight may be encouraged to lose some pounds, for example, if they have heart disease or arthritis. Patients may need a full diet or a light diet, high calorie or low fat, or low carbohydrate if they are diabetic, and all food requirements will form part of their care plan once an assessment has been made about their nutrition and hydration. The healthcare assistant might be required to help patients choose their meals from a menu, and in other cases make appropriate choices on their behalf. It would also be an important part of your role to observe any ‘nil by mouth’ instruction, for example, for patients going to the operating theatre.
It is essential that patients maintain a good level of fluid intake (hydration). Water is the most important aspect of our diet because we can’t manage without daily supplies, and fluid losses must be replaced quickly to avoid long-term damage, for example, to the brain and vital organs. The body only has a small reserve of water, and a lack of liquid intake (dehydration) results in weakness, headaches, tiredness and loss of concentration, followed by collapse and eventually death. Water losses through urine, from the skin, from breath and in faeces average about two litres per day, and they must be replaced (OpenLearn, 2016).
You may be aware of instances where patients did not receive enough hydration or nutrition which can result in devastating results:
- 'Dehydration contributes to the death of more than 800 hospital patients every year. Another 300 die malnourished̓' (Daily Mail, 2011)
- Lydia Spilner (100 years old) passed away from renal failure caused by dehydration (The Guardian, 2013).
Activity 2
(Adapted from Skills for Care (2015b) Workbook 8, Fluids and Nutrition)
Activity 3
Listen to the next audio podcast about a lady living with a visual impairment. She talks about the support she needed with eating and drinking.
Having listened to the audio podcast, write down some notes about how you would encourage a patient with a visual impairment to eat and drink.
[This audio is provided for use within the course only.]
Transcript: Support with eating and drinking
Comment
You might have said that you need to know your patient as an individual so that you’d be aware if any psychological issues are preventing them from eating (e.g. loss of dignity and independence at needing to be fed by someone else, or feeling depressed and getting no enjoyment from food), or whether the issues are practical and they physically can’t see the food (the lady speaking describes the importance of a healthcare assistant explaining what types of food are on the plate, and their positioning using a clock-face approach.) Or if she cannot see where the cutlery is you would need to hand it to her. Also she might lack the strength to lift the spoon to her mouth or simply have no appetite.
It is very important as a healthcare assistant to understand what a vital role fluids and nutrition play in patient care and recovery: wherever you work, and so you are likely to be involved in assisting patients with food and hydration each and every day.
3 Health and safety in your workplace
The Health and Safety Executive (HSE) requires employers to have a health and safety policy which sets out how they will protect everyone in their workplace, including employees, visitors, contractors and any individuals who access services. Your awareness and practice of health and safety will contribute to a safety culture at work. Accidents have causes, and steps must be taken to prevent them otherwise accidents will continue to happen.
In Section 2 you were introduced to the '6 Cs' set in place by NHS England (2012): Care, Compassion, Competence, Communication, Courage and Commitment. Competence ensures that you are keeping the individuals you support as safe as possible; only undertaking certain activities once you are competent to do so. Your workplace will have Health and Safety Representatives who are the key 'watchdog' on behalf of workers to ensure employers provide a safe and healthy workplace. Health and Safety Representatives have a legal right to carry out regular inspections and to be consulted by the employer over risk assessments and accidents or incidents at work.
The Health and Safety Executive identifies a number of health and safety risks for workers. They include:
- slips and trips in the physical environment caused by uneven floors, spilled liquids, poorly lit or unlit areas, trailing cables and wires, and so on
- musculoskeletal disorders, that is, sprains, strains and pains from lifting, carrying, pushing, pulling, reaching, repetitive movements, and so on
- stress, for example, from too much work, too many demands, conflicting demands or excessive pressure of any kind.

Now you can listen to Gail talking about some real examples of health and safety in the workplace, and what sort of incidents or accidents might occur.
Transcript: Health and safety on the ward
3.1 Infection prevention and control
As a healthcare assistant you must practise in a way that keeps the risk of transferring infection to a minimum, whether from yourself to patients or between patients. Infections and infectious diseases are caused by harmful germs, also called pathogens, such as bacteria and viruses. Most pathogens are so small that they cannot be seen without a microscope, but they are all around us.
There are a number of things you must do to prevent infections from spreading:
- prepare food safely
- carry out good hand hygiene
- make sure all equipment is cleaned properly
- dispose of waste safely
- manage laundry safely
- use personal protective equipment
- don’t go into work if you have an infectious illness.
Safe food preparation
Micro-organisms can live in food, and certain raw foods will need to be cooked to remove them. Before handling and/or preparing food, you should remove jewellery and wash your hands thoroughly. Equipment should be washed in hot soapy water between uses. Ensure food is cooked thoroughly and that food stored in a fridge is labelled, dated and kept at 5°C. Raw and cooked foods should be prepared separately. Check what precautions are taken within your workplace to ensure food poses minimal risk to your patients.
Good hand hygiene
The National Institute for Health and Care Excellence (NICE) describes five points when health and social care workers should clean their hands (NICE, 2012). These are:
- immediately before every episode of direct patient contact or care, including aseptic [cleaning] procedures
- immediately after every episode of direct patient contact or care
- immediately after any exposure to body fluids
- immediately after any other activity or contact with a patient's surroundings that could potentially result in hands becoming contaminated
- immediately after removal of gloves.
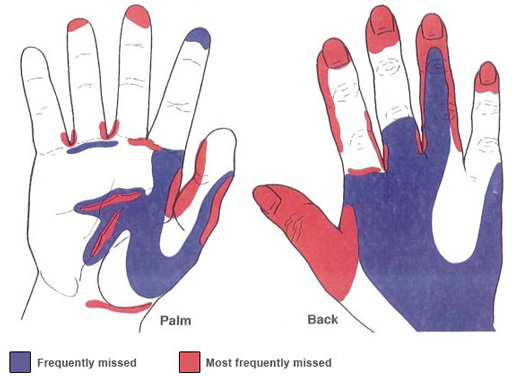
In addition, NICE (2012) defines an effective handwashing technique as involving the following three stages: ‘preparation, washing and rinsing, and drying. Preparation requires wetting hands under tepid running water before applying liquid soap or an antimicrobial preparation. The handwash solution must come into contact with all of the surfaces of the hand. The hands must be rubbed together vigorously for a minimum of 10–15 seconds, paying particular attention to the tips of the fingers, the thumbs and the areas between the fingers. Hands should be rinsed thoroughly before drying with good quality paper towels.’
When hand-washing you should remove your wristwatch and any jewellery on your hands and lower arms, and wash right up to your elbows, paying particular attention to your thumbs and the space between your fingers, areas which are commonly missed. It is also important to ensure that fingernails are clean (without nail varnish) and kept short. Remember to make use of alcohol gels supplied within your setting, and to cover any cuts you have on your hands with waterproof dressings to avoid cross-infection.
Safe disposal of waste
Clinical waste is any waste which consists of:
- human or animal tissue
- blood or other body fluids or excretions
- drugs or other pharmaceutical products
- swabs or dressings
- syringes, needles, blades (stitch removers) or other sharp instruments
Any of these could cause harm to a person coming into contact with it, and so hazardous waste must be disposed of in a way that avoids any danger or harm to yourself or other members of staff. Your workplace will have a policy about this.
Safe management of laundry
Linen that comes into contact with workers or individuals can become contaminated with harmful micro-organisms and should be washed separately from other items. Soiling is likely to include blood and tissue, sputum (a mixture of saliva and mucus), urine, vomit and faeces. Personal protective equipment (PPE) must be worn when handling infected linen as it can transfer germs to skin and clothing. Uniforms or work clothing should be changed daily and washed on a hot wash, then tumble-dried or hot ironed, to kill any bacteria present.
Correct use of personal protective equipment (PPE)
The most common PPE you will use as a healthcare assistant are disposable aprons, gloves and masks, all of which will be for single-use only. Disposable aprons protect clothing and uniforms from contamination from blood and body fluids, and you should be issued with enough uniforms for regular changing. Gloves play an important role in protecting workers from exposure to blood-borne viruses, especially where there is a risk of injury such as a puncture wound with contaminated sharps, abrasions or cuts. Masks protect you from breathing in harmful micro-organisms, and eye protection and face shields should be worn if there is a risk of being splashed with body fluids.

Activity 4
The law says that individuals should be provided with the correct materials and equipment to protect them from injury and, as far as possible, from the risk of infection while at work. If appropriate, think about occasions when you have had to wear or use PPE at work. Write down in the space below what type it was and why you had to use it.
Comment
If you already work as a healthcare assistant, there must be numerous times you’ve had to wear PPE: for example disposable aprons when bathing a patient, gloves when changing dressings and masks for surgical procedures. What does it feel like to wear PPE, and how does it make patients feel when cared for by someone wearing it?
Infectious illness
If you have cold or flu symptoms (such as coughing or runny nose), an upset stomach or skin infections, you should speak to your manager before reporting for work. If you have diarrhoea or vomiting you should not attend work until you have been free from symptoms for 48 hours.
Good hygiene is important for everybody, but as a healthcare assistant you have a duty to adopt these safe measures for your own and others’ safety.
4 Basic life support
The principles of basic life support, or first aid, are to save life by removing danger, to treat urgent symptoms and to prevent extension of injuries. You also need to avoid doing harm by carrying out treatment which you are not trained to do. Your employer should provide basic life support training. All workplaces will have a health and safety procedure to outline what to do in an emergency, and you must ensure that you are familiar with it. You must also be familiar with your patients’ care plan, for example if they are known to have any condition that could lead to sudden illness (such as a diabetic coma, or an epileptic fit), and how you should respond.
5 Awareness of mental health, dementia and learning disability
Around one in four adults has at least one mental health need at any time, and in the next 20 years the number of British people expected to suffer from dementia will grow by 40 per cent. Even though you might not be working in a setting specifically caring for people with mental health conditions, dementia and learning disabilities, it is still important to have some awareness of the signs and symptoms. This will help you to show compassion and care when you observe any behaviour that seems unusual or difficult to understand, and to be aware of the need to consult more experienced staff about behaviours if necessary.
Activity 5
The next video will raise your awareness of the needs of people with dementia. It explains certain features of the public space of a residential home especially designed for people with dementia. As you watch it, write down any points about the design that make life easier for the residents.
[This video is provided for use within the course only.]
Transcript: The Lodge: public space
The Lodge is a purpose-built residential and nursing home, designed for dementia care.
Wide, well-lit corridors are central to the dementia-friendly design.
Good design is not only about continuity, it’s also about contrast.
Comment
The building design is triangular and is based on evidence from research that people with dementia don’t do well in closed spaces, therefore it has features such as wide and well lit corridors which are a good place to walk if a resident is agitated, and in the centre is an open-plan garden space. To help the residents recognise rooms, the toilet doors are all painted bright yellow but all of their front doors are painted different colours. The dining area has a wooden floor and the carpets are plainly coloured without patterns.
The market square is good for people getting together and the whole area gives greater independence for residents, but is designed in such a way so that staff can still keep an eye on them.
The three most common types of mental health problem that you might encounter in your role are:
- depression: a common mental disorder that causes people to experience depressed mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, low energy, and poor concentration, which can be mild or very severe
- anxiety: when people cannot control their worries
- dementia: a decline in mental ability which affects memory, thinking, problem-solving, concentration and perception. This includes Alzheimer’s disease and vascular dementia.
You are probably less likely to encounter psychosis, which is when a person interprets events differently from those around them, including experiencing hallucinations, delusions or flight of ideas (MIND, 2015). It is less common and might be part of bipolar disorder (a mood disorder also known as manic depression) or schizophrenia (a psychotic disorder where people interpret reality abnormally). You might also meet patients who have a learning disability, which is where people have a significantly reduced ability to understand new or complex information and to learn new skills (Department of Health, 2001).
If you think that someone is developing symptoms of a mental health problem or dementia, or if you think that the support needs associated with their learning disability need reassessing, you should record this information and pass it on. Who you inform and how will depend on your workplace guidelines and your role. For more information on mental health, dementia or end of life care, visit the short course for carers entitled ‘Caring for adults’.
Case study: Lynne
Lynne has been managed by mental health services for many years with a diagnosis of bipolar disorder, and it has been extremely important to her to have access to the right professionals and support throughout this time. She has been fortunate in having a consistent social worker contact to help her through, who stays in touch with her on a regular three-weekly basis. They have grown to know each other well and have developed a supportive relationship. A similarly supportive relationship with her consultant has allowed for consistency of care and an understanding of her history. Lynne says that maintaining a line between the professional and patient, whilst having mutual respect and understanding of each other has been an important feature of her care. Lynne also described being treated with dignity and being allowed to grow, rather than feeling restricted by her mental health issues. During one of her bouts in hospital with depression she gained great confidence from leading a group. This is a good example of a long-term mental illness being managed effectively whilst living largely in the community through person-centred care.
What you have learned in this section
- You should always provide personalised care with due attention to the patient’s privacy and dignity.
- Fluids and nutrition will form a major part of your day-to-day work and some individuals might experience difficulties in eating or drinking without help.
- You must observe various health and safety regulations in your workplace including how to prevent infection.
- It is helpful in your role to understand the basics of mental health conditions, dementia and learning disabilities.
Further information (optional)
If you are interested in learning more about some of the mental health issues described here, the following free course is available on OpenLearn: ‘Understanding depression and anxiety’
For more information on mental health, dementia or end of life care, visit the short course for carers entitled ‘Caring for Adults’.
Section 3 quiz
Well done, you have now reached the end of Section 3 of the Introducing practical healthcare, and it is time to attempt the assessment questions. This is designed to be a fun activity to help consolidate your learning.
There are only five questions, and if you get at least four correct answers you will be able to download your badge for the ‘Your healthcare practice’ section (plus you get more than one try!).
- I would like to try the Section 3 quiz to get my badge
If you are studying this course using one of the alternative formats, please note that you will need to go online to take this quiz.
I’ve finished this section. What next?
You can now choose to move on to Section 4, Duty of care, or to one of the other sections so you can continue collecting your badges.
If you feel that you’ve now got what you need from the course and don’t wish to attempt the quiz or continue collecting your badges, please visit the Taking my learning further section, where you can reflect on what you have learned and find suggestions of further learning opportunities.
We would love to know what you thought of the course and how you plan to use what you have learned. Your feedback is anonymous and will help us to improve our offer.
- Take our Open University end-of-course survey.
References
Acknowledgements
This free course was written by Joanne Thomas (consultant for the Open University) and Emma Lipscombe (Learning and Workforce Development Officer for UNISON), with contributions from Ruth Beretta (staff tutor for the Open University).
Except for third party materials and otherwise stated (see terms and conditions), this content is made available under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 Licence.
The material acknowledged below is Proprietary and used under licence (not subject to Creative Commons Licence). Grateful acknowledgement is made to the following sources for permission to reproduce material in this free course:
Every effort has been made to contact copyright owners. If any have been inadvertently overlooked, the publishers will be pleased to make the necessary arrangements at the first opportunity.
Figures
Figure 1: © Ace Stock Ltd/Alamy
Figure 2: Food Standards Agency (http://www.food.gov.uk/)
Figure 3: © Nano/iStockphoto.com
Figure 4: (left) © iStockphoto.com/baona; (centre) © iStockphoto.com/kutaytanir; (right) © iStockphoto.com/PeopleImages
Figure 5: © unknown
Figure 6: (left) © dblight/iStockphoto.com; (right) © David FR/iStockphoto.com
Figure 7: © sturti/iStockphoto.com
Figure 8: © highway starz-photography/iStockphoto.com
Audios
‘A healthcare assistant who loves her job’ including transcript: courtesy Unison (https://www.unison.org.uk/)
‘A day in the life of a hospital ward: working with patients’ including transcript: © The Open University
‘Support with eating and drinking’ including transcript: © The Open University
‘Health and Safety on the ward’ including transcript: courtesy Unison (https://www.unison.org.uk/)
Video
Video ‘The Lodge: public space’ including transcript: © The Open University