Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 1 March 2026, 9:23 PM
Communicable Diseases Module: 6. Factors that Affect Malaria Transmission
Study Session 6 Factors that Affect Malaria Transmission
Introduction
As you learned in Study Session 5, the incidence of malaria varies from place to place and at different times. Such variations are very common in Ethiopia. There are areas where the incidence of malaria is high and other areas where the incidence is low, and some areas are malaria free. In some communities, malaria transmission lasts for several months or happens throughout the year, and in other areas it is very brief.
In this study session you will learn about the factors that affect the transmission and incidence of malaria. Climate affects the natural distribution of malaria in Ethiopia and elsewhere in the world. The three main climatic factors that directly affect malaria transmission are temperature, rainfall and relative humidity (the amount of moisture in the air). Several non-climatic factors, including differences between human hosts, human migration, and development projects, can also affect the pattern of malaria transmission and the severity of the problem.
Climatic means ‘relating to the climate’.
Understanding the climatic and non-climatic factors that affect malaria transmission will help you to understand the risk of malaria in your village better. This kind of understanding will also be useful to you in monitoring, preventing, or controlling local malaria epidemics (Study Session 12).
Learning Outcomes for Study Session 6
When you have studied this session, you should be able to:
6.1 Define and use correctly all of the key words printed in bold. (SAQ 6.1)
6.2 Describe how temperature affects the development of the parasite and the vector, and explain the association between temperature and the distribution of malaria in Ethiopia. (SAQs 6.2 and 6.3)
6.3 Explain how humidity influences malaria transmission. (SAQs 6.1 and 6.3)
6.4 Explain the relationship between rainfall and malaria transmission. (SAQ 6.4)
6.5 Describe how important non-climatic factors influence the pattern and severity of malaria transmission. (SAQs 6.5 and 6.6)
6.1 Climatic factors
Climatic factors greatly influence the pattern and level of malaria transmission in Ethiopia, in Africa and the world. The most important climatic factors that directly affect malaria transmission are temperature, rainfall and humidity. We will consider these in turn. You may find it useful first to look back at Figure 5.5 to remind yourself of the lifecycle of the malaria parasite.
6.1.1 Temperature
The ranges of minimum and maximum temperature greatly affect the development of the malaria parasite and its mosquito vector, which determines malaria transmission.
Temperature and parasite development
Temperature affects the life cycle of the malaria parasite. The time required for the parasite to complete its development in the gut of the mosquito is about 10 days, but it can be shorter or longer than that depending on the temperature. As the temperature decreases, the number of days necessary to complete the development increases for a given Plasmodium species. P. vivax and P. falciparum have the shortest development cycles and are therefore more common than P. ovale and P. malariae.
The time needed for the parasite to complete its development in the mosquito, decreases to less than 10 days as temperature increases from 21°C to 27°C, with 27°C being the optimum. The maximum temperature for parasite development is 40°C. Below 18°C, the life cycle of P. falciparum in the mosquito body is limited. The minimum temperatures are between 14–19°C, with P. vivax surviving at lower temperatures than P. falciparum. Malaria transmission in areas colder than 18°C can sometimes occur because the Anopheles often live in houses, which tend to be warmer than the outside temperature.
Temperature and mosquito development
Development of the mosquito larva also depends on temperature – it develops more quickly at higher temperatures. Higher temperatures also increase the number of blood meals taken and the number of eggs laid by the mosquitoes, which increases the number of mosquitoes in a given area.
The minimum temperature for mosquito development is between 8–10°C; the optimum temperature is 25–27°C, and the maximum temperature for is 40°C.
Altitude and temperature
As you saw in Figure 5.3 in the previous study session, altitude (elevation above sea level) is one of the most important factors that determines the pattern of malaria transmission in Ethiopia. Altitude in Ethiopia varies from 100 metres below sea level to more than 4,000 metres above sea level. Altitude influences the distribution and transmission of malaria indirectly, through its effect on temperature. As altitude increases, temperature decreases, so highlands are colder and lowlands are warmer.
In the Ethiopian highlands, with altitudes between 2,000 and 2,400 metres, malaria transmission occurs for short periods only when temperatures rise unusually high.
Can you explain why transmission occurs during these periods?
The increased temperature allows the development of parasites to occur in the mosquitoes, and the mosquito population also increases as the temperature rises.
Beyond 2,400 metres, the temperature does not go high enough to support malaria transmission and these areas are free of malaria.
Addis Ababa is free of malaria, and most of the Ethiopian highlands above 2,000 metres have little or no locally transmitted malaria (Figure 6.1). The most important reason for this is that it is generally too cold in the highlands for mosquitoes to develop in large numbers, or for the malaria parasite to develop inside the vector.

Equatorial Africa
Now look back at the map showing the distribution of malaria in Africa (Figure 5.2 in the previous study session). From your school geography education, you may remember that temperatures are higher around the equator and do not vary much through the year. Temperatures decrease progressively as you move north or south of the equator. The red part of the map shows a very high level of transmission around the equator and the light blue colour represents lower malaria transmission further north and south of the equator. One of the reasons for high levels of transmission near the equator is the warm and relatively constant temperature in tropical Africa.
6.1.2 Rainfall
As you learned in Study Session 5, anopheline mosquitoes breed in water. So the right amount of rainfall is often important for them to breed. Different anopheline mosquitoes prefer different types of water bodies in which to breed. In Ethiopia, water collections that support vector breeding appear mainly after the rains, and therefore malaria transmission is highest following the rainy season.
Note that the anopheline mosquitoes that transmit malaria do not breed in foul-smelling polluted water.
Of course, too much rainfall can flush away breeding habitats temporarily, but mosquitoes start breeding as soon as the rain stops. In most cases, flushing has a bigger impact on vector breeding habitats in the highlands and hilly areas than in the lowland plains. Not all water collections are suitable for the mosquito life cycle. In Ethiopia, rain water collections are the most important breeding ground, as the anopheline mosquitoes prefer to breed in fresh water collections created after the rainy season. Such water bodies may be clear or muddy (Figure 6.2) but they are not polluted.

There are also places where less rainfall and drought can favour mosquito breeding and malaria transmission. Such places are usually covered by vegetation throughout the year and streams and rivers often flow rapidly. When the rains fail or are delayed, the flow of streams is interrupted and pooling occurs along the stream. Pooling creates a favourable environment for mosquito breeding. Malaria vectors mainly breed in stagnant water collections, rarely in slightly moving waters and never in rapidly flowing rivers and streams.
In drier areas, rainfall can also affect malaria transmission indirectly through its effect on humidity. Vegetation cover increases after rainfall, which in turn increases the relative humidity of the environment. The effect of humidity on malaria transmission is considered below.
6.1.3 Relative humidity
Relative humidity refers to the amount of moisture in the air, expressed as a percentage; (0% humidity would mean the air is completely free of moisture and 100% humidity would mean the air is completely saturated with moisture). Relative humidity affects malaria transmission through its effect on the activity and survival of mosquitoes. You may recall that mosquitoes need to live at least 8–10 days to be able to transmit malaria.
Why is it important that mosquitoes should live this long, for the transmission of malaria?
This is the length of time required for the parasite to develop inside the mosquito host. If the mosquito dies before the parasite has developed, then transmission of the parasite cannot occur.
Mosquitoes survive better under conditions of high humidity. They also become more active when humidity rises. This is why they are more active and prefer feeding during the night – the relative humidity of the environment is higher at night. If the average monthly relative humidity is below 60%, it is believed that the life of the mosquito is so short that very little or no malaria transmission is possible.
6.1.4 Combining the effects of climatic factors
Now think of your village in terms of its suitability for malaria transmission. How many (if any) malaria cases occur each month? Does the number vary between months? When do you see the highest number? Write down the reasons you think are responsible for the variation in the number of malaria cases in your community. Then answer the following questions.
What factors do you think are responsible for the high malaria incidence in some months? Consider the following factors and decide which of them would apply to your village
- a.Immediately following the rains; if so, why?
- b.When the temperature is hot; if so, why?
- c.When the rains fail and there is drought; if so, why?
- d.When the fields are covered with vegetation; if so, why?
Of course, we don’t know the climatic pattern in your village, but malaria transmission could be high:
- a.Immediately following the rains, because there will be plenty of water collections for vector breeding after the rainy season.
- b.When the temperature is hot, because temperature speeds up vector and parasite development.
- c.When the rains fail and there is drought, because rivers and small streams slow down into pools, creating stagnant water collections for vector breeding.
- d.When the fields are covered with vegetation, because when the vegetation cover is high the humidity increases; higher humidity helps the mosquito to live longer and transmit malaria.
6.2 Non-climatic factors
Factors that affect malaria transmission, but which are not related to the climate, are called non-climatic factors. The type of vector, the type of parasite, environmental development and urbanisation, population movement and migration, the level of immunity to malaria in the human hosts, insecticide resistance in mosquitoes, and drug resistance in parasites, all have a role in affecting the severity and incidence of malaria. We will look at each of these in turn.
6.2.1 Malaria vectors

As you learned in the Study Session 5, not all mosquitoes transmit malaria – only Anopheles mosquitoes (Figure 6.3) can carry the malaria parasite. In Ethiopia there are about 40 different species of Anopheles mosquitoes, but only four of them are known to transmit malaria parasites, and just one of them, Anopheles arabiensis, is responsible for more than 95% of malaria transmissions.
Different species of Anopheles mosquitoes differ in their capacity to transmit malaria. This depends on the biology and behaviour of the mosquitoes. Mosquitoes in the Anopheles gambiae group (which includes A. arabiensis), are the most efficient malaria vectors in the world. These mosquitoes are found only in Africa. In fact, the higher incidence of malaria in Africa compared to other parts of the world is mainly due the efficiency of these mosquitoes in transmitting the parasites.
Mosquitoes need a blood meal to develop and reproduce. They can take their blood meal either from humans or animals. Mosquitoes that mainly feed on humans are more efficient carriers of malaria than those that feed on animals.
One reason why mosquitoes in the A. gambiae group are very good vectors of malaria is that they prefer to bite humans more than animals. Mosquitoes that feed on humans and animals equally are much weaker vectors of malaria. Others feed exclusively on animals and are not malaria vectors. Therefore, the type of Anopheles mosquitoes and their feeding behaviour influence the intensity of transmission in an area.
Your knowledge and practical skills in identification of important breeding habitats in your village will be very helpful in your malaria prevention activities.
Mosquitoes adapted to breeding close to human settlements, and able to breed in a wide range of environments, are also better vectors of malaria than mosquitoes that breed away from human habitation. Some mosquitoes breed in small pools that are partially or completely exposed to the sun, while others prefer to breed in shaded stagnant pools. A. gambiae mosquitoes breed in a wide range of habitats, including small water collections such as hoof-prints, water-filled holes in rocks and trees, as well as dams, river beds and lake shores. Because A. gambiae vectors can breed in so many different habitats, they are responsible for much of the malaria transmission in Africa.
The main vector of malaria in Ethiopia, A. arabiensis, can be found in a variety of water collections, mainly closer to human habitations. However, stagnant water collections in borrow pits, ponds, micro-dams, pools in small rivers, and streams created immediately after the rainy season, are the most important breeding habitats for this vector.
6.2.2 Malaria parasites
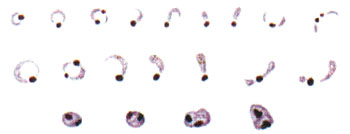
You learned in Study Session 5 that there are four types of malaria parasite that can infect people. They are single-celled protozoa that can only be seen if viewed under a microscope (Figure 6.4).
Can you recall the two forms of malaria that are most common in Ethiopia, and which one of them is more dangerous?
P. vivax is responsible for around 40% of cases and P. falciparum is responsible for around 60% of cases of malaria in Ethiopia. P. falciparum causes the most dangerous type of malaria and often kills untreated patients. P. vivax (and the other two rare forms) can make people very sick, but are not usually killers.
In some areas of Ethiopia falciparum malaria is more common, while in other areas vivax malaria is more common. Falciparum malaria is more common in Africa than in other parts of the world, and this is one reason why there are more deaths from malaria in Africa than elsewhere.
6.2.3 Water development projects
Big and small water-related development projects, such as irrigation channels, dams and ponds, can increase the incidence of malaria in villages that are located near such projects.
How can water development projects affect malaria transmission?
They create more vector breeding habitats; more vectors mean more malaria transmission.
You will learn about environmental management to reduce the breeding sites for mosquitoes in Study Session 9 of this Module.
Agricultural development, particularly with the use of irrigation, creates breeding sites for malaria mosquitoes, leading to increased malaria transmission. For instance, the use of irrigation to flood agricultural land during rice cultivation has long been associated with an increase in the number of vectors and a corresponding increase in the burden of malaria. Irrigated farming and rice agriculture is becoming more common in the lowlands of Ethiopia.
6.2.4 Urbanisation
The incidence of malaria is generally lower in urban areas than in rural areas. There are a number of reasons for this:
- While there is plenty of space for vector breeding in rural villages, mosquito breeding sites in urban areas are limited because more space is covered by houses.
- The main vectors of malaria in Ethiopia and elsewhere in Africa, are mosquitoes in the A. gambiae group, which breed in clean water; most water collections in urban settlements are polluted and unfavourable for mosquito breeding.
- People in urban areas may have more access to health care and malaria prevention strategies than people in rural villages.
However, rapid urbanisation of areas within or on the outskirts of urban centres is commonly done in an uncontrolled fashion without thought or planning (Figure 6.5). The settlers are mainly migrant workers from rural villages. Conditions are crowded; housing is often of poor quality or is of temporary construction; and the provision of health care and sanitation is often inadequate.

Settlers tend to dig several pits to extract stone and soil for house construction, creating numerous breeding grounds for mosquitoes. This can lead to explosive growth of mosquito vectors, increased exposure of the population to vectors due to poor housing, and amplification of disease to epidemic proportions through lack of effective treatment.
Your main responsibility as a rural Health Extension Practitioner is mainly to provide care and set up preventive measures in rural communities. However, some semi-urban settlements at the periphery of urban centres could fall under the rural classification and be part of your catchment area. Remember that people living in such semi-urban centres can be at a higher risk of malaria than typical rural communities.
6.2.5 Population movement and migration
Population movements have significant implications for malaria transmission. The majority of the population movements in Ethiopia involve people moving from the highlands to the malaria-endemic lowlands as seasonal labourers. These people are often employed as daily labourers in the crop fields during the planting and harvesting seasons (Figure 6.6), when malaria transmission is at its peak. The poor living conditions and inadequate health care in such agricultural projects often worsen the problem of malaria. Migrants from malaria-free highlands lack immunity against the disease, as well as the appropriate knowledge of the transmission process and how to avoid being bitten by mosquitoes.

Migration for the purpose of permanent settlement in a new area is also common in Ethiopia and is a major factor associated with malaria transmission. Migration is often from densely populated highlands to malaria-endemic lowlands, where the population density is low and the soil is more fertile. Major environmental transformations like deforestation, and new construction etc, take place during resettlement, enhancing the proliferation of mosquito breeding sites, and resulting in major malaria outbreaks.
Population movements and migration also make the malaria problem worse in the areas from which the migrants came. Temporary migrant workers often bring the parasites back to the malaria-free highlands and local transmission can be readily established as many of these communities could support vector breeding. Such sporadic epidemics could affect a large number of people, as the population in malaria-free areas is generally non-immune.
You will learn about drug-resistance when we describe malaria case management in Study Session 8.
Large population displacements can also occur rapidly due to causes like war and civil unrest, or natural causes like drought and famine, flooding and earthquakes, etc. Displaced people from areas with malaria can introduce or reintroduce malaria into areas that are malaria free, and in some cases spread drug-resistant malaria. Displaced populations can in some cases be at a higher risk of getting sick or dying from malaria because:
- Displaced people may not have proper housing.
- They often camp near water bodies that serve as mosquito breeding sites.
- They could be non-immune, if moving from malaria-free to malaria-endemic areas.
- Malnutrition can worsen the malaria problem.
- The health care system can be overburdened, so there may be very limited malaria care and preventive measures.
Though the chance of large scale population displacement due to social and natural disasters is rare in Ethiopia, it is important for you to keep in mind that displacement can worsen the problem of malaria.
6.2.6 Human host factors
Differences in human hosts also affect the pattern of malaria transmission and the severity of the disease. When it comes to malaria, people are either immune, or non-immune. Immune people often have a better chance of tolerating the effects of malaria and surviving the disease than non-immune people. In highly endemic areas, children under five years of age and pregnant women are the most at risk (Figure 6.7), because they have weak immunity to malaria infection. Immunity to malaria develops slowly after several infections and children need at least five years to develop their immunity. Pregnant women have less immunity to malaria due to their pregnancy.

Certain population groups can be infected by some types of malaria parasites, but not by others. For example most Africans south of the Sahara can get infected by falciparum malaria, but not by vivax malaria. This is another reason why most of the disease and deaths due to malaria occur in Africa, because falciparum malaria is the deadliest form of malaria and is highly prevalent in the continent.
6.2.7 Insecticide resistance in vectors
In Study Sessions 9, 10 and 11, you will learn how some insect-killing chemicals (insecticides) are used to kill mosquitoes and protect communities from mosquito bites. No (or low numbers of) mosquito bites mean no or less risk of malaria. However, after repeated application of these chemicals, the mosquitoes develop insecticide resistance, which means that they are no longer killed by the insecticides. This means a large number of mosquitoes will survive in the community, and the risk of malaria infections rises and many people can be affected.
6.2.8 Drug resistance in malaria parasites
You will learn about the medicines used to treat malaria in Study Session 8. These drugs kill the malaria parasite inside the human body. However, similar to the insecticide resistance mentioned above, after repeated use of an anti-malaria medicine, the parasite can develop resistance to that particular drug or to similar medicines. As a result, the parasites inside the human body can no longer be killed and patients cannot be cured unless new drugs are developed for treatments. If drug-resistant malaria parasites are not cleared by treatment from infected individuals, they are easily picked up by vector mosquitoes, and transmitted to new susceptible individuals who then develop drug-resistant malaria. Moreover, more people who are not getting cured by drug treatment means that more will die of malaria.
6.2.9 Interruption of control and prevention measures
Malaria is a curable disease if the parasites remain susceptible to available treatments, and it can be prevented by using several methods. However, long-term and sustained implementation of prevention and control measures is necessary to significantly reduce or eliminate the problem from a country or a specific geographic area. As a result of long-term successful interventions, a local population can lose their immunity to malaria in an area where it has been reduced to a low level for some time. Remember that repeated infections are necessary to develop immunity to malaria. Immunity gets lower or is lost if a person moves out of a malaria endemic area, or is protected from infection for several years. Therefore, if control and preventive measures are stopped before the disease is eliminated, malaria can surge back and affect more people, and affect them more severely than before.
Summary of Study Session 6
In Study Session 6, you have learned that:
- Malaria transmission is directly affected by different climatic factors.
- There is an optimal range of temperature that is best for the development of the vector and the parasite.
- Temperature greatly influences the distribution of malaria in Ethiopia; most highlands in Ethiopia have very little or no malaria due to low temperature.
- Altitude is the most important factor that determines the distribution of malaria. Altitude and temperature are closely related in Ethiopia. Lowlands are warm (good for malaria transmission), highlands are too cold for malaria parasites and vectors to develop.
- Higher humidity makes the vector live longer; malaria is transmitted by vectors that live 8–10 days so the parasites have time to develop.
- The main malaria transmission in Ethiopia is after the rainy season because rainfall creates many vector breeding grounds.
- Several non-climatic factors affect the severity and incidence of malaria transmission, including the type of vectors and parasites, environmental developments and urbanisation, population movement and migration, the level of immunity in the human hosts, insecticide resistance in mosquitoes, and drug resistance in parasites.
Self-Assessment Questions (SAQs) for Study Session 6
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 6.1 (tests Learning Outcomes 6.1 and 6.3)
Imagine that the relative humidity of your village is 40% in February and 80% in September. Describe how this could affect malaria transmission in your village. Start by explaining the effect of humidity on the vector.
Answer
There will be malaria transmission in September, but not in February. At 40% humidity, mosquitoes cannot live long enough to transmit malaria in February.
SAQ 6.2 (tests Learning Outcome 6.2)
Imagine that the average daily temperature in your village is 12°C and you rarely see malaria cases. Describe the reason why there is no malaria transmission in your village.
Answer
A daily average temperature of 12˚C is not enough for the parasites to develop inside the mosquito vector. It is too cold.
SAQ 6.3 (tests Learning Outcomes 6.2 and 6.3)
Imagine that your village is located at 1,000 metres above sea level and is covered with vegetation throughout the year. Several new malaria cases are occurring every month. What could be the factors causing the high malaria rate in your village?
Answer
- Located at 1,000 metres above sea level, your village will have favourable temperatures for mosquito growth and parasite development.
- High vegetation coverage increases humidity and high humidity helps the vector to live longer; malaria is transmitted by long-living vectors.
SAQ 6.4 (tests Learning Outcome 6.4)
Most of the malaria cases in your village come in the two months following the rainy season. Very few cases occur in the dry season. Explain the reason why so many cases occur after the rainy season.
Answer
The rains create several vector breeding grounds; many vector breeding sites produce many vectors; more vectors mean more malaria transmission.
SAQ 6.5 (tests Learning Outcome 6.5)
Anopheles arabiensis prefers to bite humans more than animals. Another Anopheles mosquito, An. pharoensis, feeds more on animals than humans. Which one of them will be a better vector of malaria and why?
Answer
- An. arabiensis will be a better vector of malaria.
- Mosquitoes that prefer to feed on humans have a better chance of picking up the parasite from an infected person and transmitting it to another person.
SAQ 6.6 (tests Learning Outcome 6.5)
In village A, most of the malaria cases are due to falciparum malaria. In village B, vivax malaria is more common than falciparum malaria. Which village will have more deaths due to malaria and why?
Answer
- Village A will have more deaths due to malaria than village B.
- Falciparum malaria is the more dangerous form of malaria that often causes deaths; people very rarely die of vivax malaria.