Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 19 April 2024, 2:02 PM
Communicable Diseases Module: 11. Malaria Prevention: Insecticide Treated Nets
Study Session 11 Malaria Prevention: Insecticide Treated Nets
Introduction
In Study Sessions 9 and 10 you learned about two important malaria prevention methods targeted at malaria vectors: killing mosquito larvae as they develop in water, and using IRS to kill adult mosquitoes that enter houses to bite people. In this study session, you will learn about another malaria prevention strategy directed against adult mosquitoes, which is widely used in malaria risk areas: the use of insecticide-treated nets (ITNs). An ITN is a mosquito net impregnated with insecticide that repels, disables or kills mosquitoes coming into contact with it.
An important part of your responsibility is distributing ITNs to the community and maintaining high coverage through replacement of damaged nets, sustained coverage of people at risk, educating households on how to hang the nets, how to use them properly and consistently, and how to repair them when damaged. In this study session you will learn the objectives of using ITNs for malaria prevention, and about methods of effective net distribution, replacing old nets and monitoring their use. It will help you understand your role in the ITN programme, including what you need to do to make sure people in your community benefit fully from using ITNs.
The skill and knowledge you obtain from this study session about ITNs as a malaria prevention strategy will help you ensure that people in your community get the maximum benefits from the nets distributed. Like other malaria control and prevention tools, ITNs protect people from malaria and save lives.
Learning Outcomes for Study Session 11
When you have studied this session, you should be able to:
11.1 Define and use correctly all of the key words printed in bold. (SAQ 11.1)
11.2 Discuss the principles of bed net use in malaria prevention. (SAQs 11.2 and 11.3)
11.3 Describe the different mechanisms of net distribution. (SAQs 11.4 and 11.5)
11.4 Explain the importance of correct and sustained net use and the mechanisms for monitoring your local ITN programme. (SAQs 11.6 and 11.7)
11.1 ITNs as a malaria prevention tool
Insecticide treated nets (ITNs) are one of the most effective methods of preventing malaria in malaria-risk areas. The insecticides used for treating bed nets kill mosquitoes, as well as other insects, and they also repel mosquitoes, reducing the number entering the house to feed on the people inside. In addition, if high community coverage of ITNs is achieved, the numbers of mosquitoes, as well as their life span, will be reduced. When this happens, all members of the community are protected, regardless of whether or not they are using a bed net. To achieve such effects, high community coverage is required. The use of ITNs has repeatedly been shown to reduce the incidence of severe disease and mortality due to malaria in malaria-affected regions. ITNs can also have a beneficial effect on other insect pests, such as head lice, ticks, bedbugs and cockroaches.
11.1.1 How ITNs work
Mosquito nets fall into two groups: those that are not treated with insect killing or repelling chemicals, and those that are treated with such chemicals (i.e. ITNs). All mosquito nets act as a physical barrier, preventing bites by vector mosquitoes and thus providing personal protection against malaria to the individual(s) using the nets. In addition, ITNs can kill or disable mosquitoes by contact with the insecticide.
ITNs are most useful when a large proportion of biting by local mosquitoes takes place after people have gone to sleep inside houses. ITNs have three main functions:
- ITNs (like all nets) reduce contact between the person and mosquito by acting as a physical barrier.
- When mosquitoes are in contact with the ITN, the insecticide on the nets kills them.
- The insecticide on the nets also has a repellent effect, that is, it prevents mosquitoes from coming close to a person sleeping under ITNs, and to some extent it prevents mosquitoes from entering and staying in a house. The repellent effect adds a chemical barrier to the physical one, further reducing human–vector contact and increasing the protective effect of the mosquito nets.
Individuals sleeping under ITNs have effective personal protection against malaria vectors. However, if ITN use is widespread in a village or community, it can actually increase protection against malaria vectors even for those who are not sleeping under nets.
Can you explain why widespread ITN use in a community could increase protection against malaria vectors even for people who are not sleeping under ITNs?
ITNs can kill mosquitoes on contact. For this reason, if ITN use is widespread, the local malaria vector population will be reduced, so even people who do not have ITNs will be less likely to be bitten by a malaria vector.
Thus ITNs can be a very effective vector control intervention for reducing malaria transmission for individuals and communities.
11.2 Types of ITNs
Pyrethroids are the only family of insecticides used to treat bed nets, as they are safe to humans. Nets requiring re-treatment every six months are no longer used in malaria control programmes in Ethiopia or elsewhere. Therefore, the term ITN in the rest of this study session refers to LLINs.
There are two types of ITNs: conventionally treated nets and long-lasting insecticidal nets or LLINs. A conventionally treated net is a mosquito net that has been treated by dipping in a pyrethroid insecticide. Dipping is often done at the village level, by health workers or communities themselves. However, to ensure its continued insecticidal effect, the net needs to be re-treated after three washes, or at least every six months. A much better alternative is the long-lasting insecticidal net. LLINs are factory-treated mosquito nets made with a netting material that has insecticide incorporated into the fibres, or as a coating on the fibres. LLINs are effective against mosquitoes for at least 20 standard washes, or three to five years under field conditions. As the lifespan of most nets is three to four years, the insecticides in LLINs remain effective for the whole life of the net. Therefore, there is no need to re-treat LLINs.
11.3 Mosquito net models
Mosquito nets are produced in different sizes and shapes. A net should cover the sleepers completely and should cover sufficient space for them to avoid contact with the fabric. Sufficient length is needed so that the net can be tucked in under the mattress or sleeping mat. Different models have been developed for different situations. They differ in convenience for daily use, and prices vary widely. The method of suspension is an important consideration.
11.3.1 Rectangular nets
The rectangular net (Figure 11.1) is normally used over a bed or sleeping mat. It is the model widely used in Ethiopia. It is suspended from four or more loops along the upper edges.
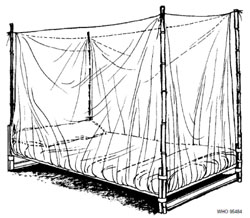
Dimensions vary: most nets have a height of about 150 cm and a length of 180–190 cm. A single-size net has a width of 70–80 cm, contains about 9 m2 of netting material and is used to cover one person on a single bed or sleeping mat. Double nets with a width of 100–110 cm (10–11 m2 of netting) and family-size or large double nets with a width of 130–140 cm (12–13 m2 of netting) are used for larger beds. The optimal size depends on sleeping habits and available space. All nets distributed in Ethiopia are family size nets.
Special supports for rectangular bed nets
Indoor supports: Where it is customary to rearrange and use beds for seating during daytime, nets should be supported using detachable poles or mosquito net supports attached to the ceiling or walls.
If possible children should go to sleep as early as possible indoors under nets; if they have to sleep outdoors they must sleep under nets.
Outdoor supports: In some villages where the climate is hot, people tend to sleep outdoors during the peak malaria season. People may also stay late outdoors working or chatting before going indoors to sleep. In many cases, people let their children sleep outdoors until the adults go indoors to sleep late at night. Where people usually sleep outdoors, or stay outdoors late into the night during the hot season, nets should be used outdoors. Outdoors, nets are best supported by a frame that can be easily detached from the bed (Figure 11.2). Most vectors of malaria bite people from sunset to dawn. To get full protection from the nets, people must use nets from dusk to dawn. If people stay late outdoors chatting, they should use the nets outdoors too. In particular, children should not be left to sleep outdoors without nets.

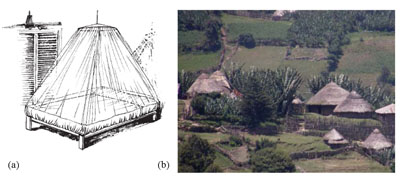
11.3.2 Circular nets
Circular, or conical, nets are sometimes preferred because they can be hung from a single support (Figure 11.3a). The nets are mostly available in double size. Compared with the rectangular net, more care has to be taken to avoid contact between the body and the net, which would allow mosquitoes to feed. Circular nets could be better suited to circular houses with limited space, which are very common in Ethiopia (Figure 11.3b).
11.4 Deciding the number of ITNs per household
The first step in ITN programmes is making the nets available to the community. Several methods have been tried to make ITNs available to a large number of people in malaria-risk areas. They included encouraging people to buy nets from the market at full price, making nets available at subsidised or reduced prices, and credit schemes.
However, none of these methods was effective in scaling up coverage of nets in poor communities like those in rural Ethiopia. Therefore the current policy of the malaria programme in Ethiopia is to distribute nets free of charge to all population groups, using the methods described in Section 11.5 of this study session.
The objective is to ensure that communities living in malaria-risk villages have enough nets to cover all sleeping sites in the household. In Ethiopia, the strategy since 2005 has been to provide, on average, two ITNs per household in all malaria-risk areas. Between 2005 and 2007 this strategy provided access to ITNs to an estimated 10 million households, or approximately 50 million people, living in malaria-risk areas.
Approximately how many ITNs were distributed in Ethiopia between 2005 and 2007?
10 million households received ITNs. Households received on average two ITNs per family; so around 20 million ITNs were distributed.
Although an average of two ITNs per household is used for logistical or planning purposes, it does not mean that every household will get two nets. The number of ITNs a household will receive depends on family size, and is based on the general principles shown in Table 11.1.
| Family size | Number of ITNs to be supplied |
|---|---|
| 1 to 2 | 1 |
| 3 to 5 | 2 |
| 6 to 7 | 3 |
| More than or equal to 8 | 4 |
The number of sleeping sites in the household must also be taken into account during distribution of the nets. For example, even if there are only two people in the household, if they sleep separately in two different sleeping sites, the household needs two nets — not just one as indicated in Table 11.1. You must also make sure that pregnant mothers and children under five years old always get priority access to ITNs, even if this means supplying extra ITNs to the household.
Why should children and pregnant mothers get special attention during ITN distribution?
Because children and pregnant mothers are at higher risk of getting ill and dying of malaria (Study Session 6).
11.5 Methods of ITN distribution
There are two main methods of supplying nets to the community and maintaining high coverage. One is mass distribution, which is termed catch-up distribution of nets. This is a method used to achieve coverage of the entire community, or of target groups, as quickly as possible. The other method is termed keep-up distribution of nets. This is a method employed to maintain the coverage achieved by mass distribution by replacing nets as needed and providing nets for newcomers and newborns in a community.
There are a number of advantages of distributing ITNs through the Health Extension Programme under your supervision:
- ITN distribution is integrated into the existing health system, instead of relying on special campaigns.
- All malaria-risk villages of 5,000 people should have at least two Health Extension Workers or Practitioners like yourself deployed close to the community. Your knowledge of the customs and culture of your community will be very helpful in increasing the acceptability and use of ITNs. You will also have first hand information about family size and the number of sleeping sites in each household, which determines the number of nets needed in your community (as in Table 11.1).
- Through your activities, ITNs can quickly be replaced or supplied as needed, ensuring continuous access to ITNs (summarised in Box 11.1). This should reduce the proportion of people in your community remaining uncovered due to damage or loss of nets, and ensure that additional nets are available for pregnant mothers and newborn babies.
- Planning the requirement of ITNs for continuous replacement and additional distribution can be based on precise information collected by community-based health workers such as yourself, so it is more likely to reflect ITN requirements accurately.
Box 11.1 Health Extension Programme activities in ITN distribution in malarious villages
You are expected to perform the following activities in order to effectively and efficiently undertake ITN distribution in your village:
- Determine the number of households in your village.
- Determine the average family size in your village (the total number of people in your village divided by the total number of households in the village).
- Prepare a record of the number of people in each family and if possible the number of sleeping sites in each household.
- Submit your plan, including the above data, to the District Health Office.
- Discuss with community leaders and elders, and with community health workers, how to distribute the nets as quickly as possible, and involve them in distribution of the nets.
- Transport the required number of nets from the District Health Office to the health post.
- Arrange temporary storage of the ITNs.
- Train community health workers on procedures of ITN distribution and the key messages about proper and consistent use, which they should communicate to the households during ITN distribution.
- Always give priority to children under five years old and pregnant women, when there are not enough nets to cover the whole population. Pass the message to the households about prioritising the nets to protect their young children.
- Distribute nets as soon as they arrive at the health post.
- Consider distributing the nets through house-to-house visits, as this will be the best way to assist the households with hanging the nets and teaching them the proper use of the nets.
- Ask households to remove badly damaged nets, tear them down to be used as window screens or put them under the mattress or mat to kill other pests, like bedbugs. Never allow households to keep using damaged old nets while keeping new nets unused.
- Always unpack nets before handing them to beneficiaries.
- Convince households to repair damaged nets promptly, to extend their useful life.
The following are different ITN distribution mechanisms that you have to know to do your job effectively. Remember that appropriate mechanisms of nets distribution and replacement should be discussed with your supervisors at the health centre and District Health Office. The choice of distribution and replacement methods depend on the availability of nets at Regional and District levels.
11.5.1 Mass distribution (catch-up) of nets
A variety of methods are available to distribute ITNs to a whole community, as described below.
ITN distribution via house-to-house visits
The best way to distribute ITNs in the community is to visit every house to distribute them. In this way you can ensure that:
- The nets are given to the right people.
- The nets are hung up and not left in their packages.
- The nets are hung properly.
- People get information about how to hang and use the nets outdoors, if outdoor sleeping is common in the village.
- Non-functional old nets are removed and used for other purposes.
- People receive face-to-face education on the benefits of proper and consistent use of ITNs, including the benefits of putting children under nets as early as possible at night.
However, the problem with house-to-house distribution is that it is time-consuming, so it might take you and your colleagues a lot of time to visit 1,000 or so households. To overcome this problem, you should train volunteer community health workers and village leaders to help with the mass distribution of the nets via house-to-house visits.
Stand-alone ITN distribution campaigns
ITNs can also be distributed to all households in the village that need them by inviting people to come to central distribution points, where households are given ITNs based on the village register. At the same time, education and demonstrations can be given collectively to a large number of people. The advantage of this kind of distribution is that a large number of nets can be distributed quickly. However, the health education messages and practical demonstrations may not be adequately communicated to individuals (Figure 11.4).

Distribution integrated with immunization or outreach campaigns
ITNs can also be delivered through the systems and organisations used to deliver immunization, so immunization and ITNs can be delivered at the same time. ITN distribution can also be linked to the other outreach services such as the structure used to deliver bi-annual vitamin A supplements, de-worming, and nutrition screening campaigns.
The disadvantage of linking ITN distribution to immunization and other outreach programmes is that only households with young children (one to five years old) are targeted by these programmes, so other households will not be covered. In fact, such distribution methods are not generally recommended in Ethiopia, as the country has strong community-based health delivery systems, such as the Health Extension Programme, of which you are a part.
11.5.2 Replacement or ‘keep-up’ distribution
As you learned above, the aim of ITN distribution in Ethiopia is to protect everyone living in malaria-risk areas, so every effort is made to achieve 100% coverage of all people living in malaria-risk villages.
After the initial distribution of ITNs to as many people as possible via ‘catch-up’ campaigns, you need to maintain high coverage continuously, so as many people as possible remain protected and the disease can be controlled. Such follow-up distribution of ITNs is known as ‘keep-up’ distribution, and it is necessary because:
- Currently the ITNs used for malaria prevention are only functional for three to four years. After three to four years, the ITNs become damaged and have to be replaced by new ones. Nets can also be torn or damaged before three to four years, for a variety of reasons. You should replace any damaged nets regularly to keep the coverage high.
- Mothers who become pregnant after the ‘catch-up’ distribution may move to their own sleeping site separate from other family members and may need to be provided with their own ITN. Giving ITNs to all pregnant mothers attending antenatal care (ANC) will keep them protected from malaria. This could also serve as an incentive for mothers to attend ANC, where attendance in rural Ethiopia is generally low.
- Newcomers to a village and newborns will need additional ITNs.
11.6 Proper and sustained use of ITNs
To give the required protection, ITNs need to be used properly and regularly. One of the biggest challenges for the ITN programme in Ethiopia, and in many other African countries, is to ensure proper and consistent use of ITNs. A malaria indicator survey (MIS) conducted in Ethiopia in 2007 showed that, despite a national ITN coverage rate of 68% of households in malaria-risk areas, less than 50% of the people who have nets slept under an ITN. The MIS results also showed that many people do not understand how malaria is transmitted, or why ITNs are important for malaria prevention.
Understanding how malaria is transmitted, and why it is important to sleep under ITNs, is important for people to change their behaviour. This needs education. Mass media and education materials such as posters and banners can provide information and create awareness about the need to use ITNs correctly. Personal messages from you are even more effective.
11.7 The role of the health worker in education about ITNs
Health workers at all levels of the health system need to try and make sure that ITNs are used properly by the community. However, as a locally-based Health Extension Worker or Practitioner you are the person in the best position to make a significant difference, by educating and convincing the people in your community to use ITNs properly and consistently. The success or failure of the ITN programme depends on your efforts to make people aware of the benefits of ITNs, and to change their behaviour so they use ITNs properly. Please consult your supervisors at the health centre and District Health Office if you face any problems in this regard.
Using CHWs effectively is covered in the Module on Health Education, Advocacy and Community Mobilisation.
Many health posts now also have a network of volunteer community health workers (CHWs) to support you in community-based activities. You need to use these CHWs to help you increase contact with each household in a more organised way, in order to increase the use of ITNs in your village.
Misuse of ITNs by community members, for example for covering hair, for fishing and for carrying goods, should be identified and discouraged. Not sleeping under ITNs consistently, or sleeping outdoors without ITNs (whether for adults or children) needs to be addressed if they are part of the problem. Some people may also be selling their nets.
Multiple contacts and one-to-one interactions are known to be important in bringing about changes in behaviour.
11.8 Monitoring ITN utilisation
Continuous monitoring of the possession and proper use of ITNs is also very important if ITN programmes for preventing malaria are to be successful. You should visit a sample of households regularly and check:
- Whether all the nets you gave the family are physically present in the household.
- Whether the nets have been hung properly (Figure 11.5).
- Whether everyone in the household slept under the nets the previous night.
- The physical condition of the nets and advise the family to repair minor damage.
- The names of the family members who sleep under each net.
- If possible ask them what time children under five years and adults normally go to sleep in the evening; advise alternative solutions if outdoor sleeping or staying out late is an issue.
- Address any concerns or problems about net use from the household.

As a health worker providing antenatal care (ANC) and immunization services to the community, you should always ask pregnant women at every ANC visit, and parents of children at all vaccination visits, whether they have nets and whether they are using them properly. You should check if the mothers and their children slept under ITNs the previous night, and you should record their responses on the Expanded Programme of Immunization (EPI) monthly form.
As you learned from this study session, the most important components of an ITN programme in malaria prevention are distributing the ITNs correctly, maintaining high coverage, educating people on proper and consistent use, and monitoring their utilisation. You are the key person who can effectively implement all the above activities and protect people from malaria-related illnesses and deaths.
Summary of Study Session 11
In Study Session 11, you have learned that:
- ITNs are one of the most important malaria prevention methods and are widely used in Ethiopia.
- ITNs provide personal protection for individuals who use them properly.
- When coverage with ITNs is high, they can provide community protection by killing a large number of mosquitoes trying to feed on humans.
- To achieve high coverage, ITNs need to be distributed to the community free of charge.
- The most effective way to distribute ITNs is through house-to-house visits; however other methods can also be used (e.g. stand-alone campaigns).
- You are the most important person in planning and undertaking distribution of nets to the community.
- Volunteer community health workers and village leaders can support ITN distribution campaigns in the village.
- Keeping coverage high through replacement of damaged nets, and distributing new ones to people in need, is important for effective community protection.
- Proper and consistent utilisation of nets is important for ITNs to be effective.
- Educating people on proper and consistent use of nets and monitoring behaviour change is one of your most important tasks in the ITN programme.
Self-Assessment Questions (SAQs) for Study Session 11
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 11.1 (tests Learning Outcome 11.1)
Sleeping under an insecticide treated net (ITN) protects people from getting malaria. Which of the following statements about ITNs is false? In each case, explain what is incorrect.
A ITNs protect people from malaria by killing the malaria parasites.
B ITNs do not kill mosquitoes that come in contact with the nets.
C ITNs can repel mosquitoes from coming closer to people sleeping under nets.
D ITNs have chemicals in (or coated onto) their fibres, which can kill mosquitoes.
E The chemical on ITNs kills only mosquitoes.
F The chemicals coated on ITNs are harmful to humans.
Answer
A is false. ITNs protect people by killing or repelling the mosquitoes (not the parasites).
B is false. ITNs do kill mosquitoes that come in contact with the nets.
C is true. ITNs can repel mosquitoes from coming closer to people sleeping under nets.
D is true. ITNs are impregnated with chemicals that kill mosquitoes.
E is false. ITNs also kill other household pests like bedbugs that come in contact with the nets.
D is false. The chemicals used to treat nets are harmless to humans and animals.
SAQ 11.2 (tests Learning Outcome 11.2)
Describe the difference between non-treated and insecticide-treated nets (ITNs).
Answer
Non-treated nets have no chemicals, so they cannot kill mosquitoes and other insects. Treated nets do have insecticides coated or incorporated into them. Untreated nets only act as physical barriers against mosquito bites, while ITNs can also kill or repel mosquitoes.
SAQ 11.3 (tests Learning Outcome 11.2)
What is the difference between regularly/conventionally treated nets and long lasting insecticidal nets (LLINs)?
Answer
Conventionally treated nets have to be dipped in chemicals every six months or after three washes; LLINs have chemicals in them that remain effective for the life of the nets (three to four years).
SAQ 11.4 (tests Learning Outcome 11.3)
Different methods are used to distribute nets to communities. State two important mechanisms of mass net distribution, in each case with their advantages and disadvantages.
Answer
- House-to-house visits: The advantage is that these visits ensure that nets are given to the right people and effective face-to-face education on net use is provided. However, it can take a lot of time to distribute nets to all households in this way.
- Inviting people to come to the health facility or other central location in the village: this is a good method to distribute a lot of nets rapidly. However, education about using the nets may not be effective as it is given to everyone and some individuals may not understand or accept the messages.
SAQ 11.5 (tests Learning Outcome 11.3)
What methods can you use to keep coverage of nets high in your community, after they have been distributed by mass (catch-up) methods?
Answer
- Giving nets to pregnant mothers during antenatal care visits
- Giving nets to children during immunization visits
- Giving nets to newcomers to the village
- Giving nets to replace old or torn nets.
SAQ 11.6 (tests Learning Outcome 11.4)
One of the most important challenges in ITN programmes is a low rate of net utilisation. State at least two behaviours of people that are not considered to be proper use of nets.
Answer
At least two of the following:
- Not sleeping under nets.
- Using nets for fishing or other purposes.
- Selling them.
- Not hanging nets properly.
- Not using nets for sleeping outdoors.
SAQ 11.7 (tests Learning Outcome 11.4)
High net coverage is expected to protect people from malaria and reduce the incidence of new cases. Imagine that, in spite of high net coverage in your village, many people are getting infected with malaria and coming to your health post for treatment. What could be the possible explanation for this problem?
Answer
- A large number of people are not sleeping under their nets.
- Many people are sleeping under nets, but too late in the night, after mosquitoes have already begun to feed on humans.
- Many of the nets are old and damaged.