Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Sunday, 8 March 2026, 10:28 AM
Health Management, Ethics and Research Module: 16. Extended Case Study on Health Management, Ethics and Research
Study Session 16 Extended Case Study on Health Management, Ethics and Research
Introduction
This final study session is rather different from the previous study sessions in this Module. It is based on one extended case study, which has been designed to help you think more about all the issues that you have been learning about in the rest of the Module. Ethiopia is such a large and diverse country that no single case study can reflect precisely the situation that you will come across in your work as a Health Extension Practitioner. However, the case study that follows includes examples of many of the situations that you will encounter wherever your work takes place. It highlights the work of an imaginary Health Extension Worker called Alemitu, who has to deal with many of the management, ethical and data collection issues that Health Extension Workers and Health Extension Practitioners routinely face in their working lives. In this case study, we focus on health issues relating to immunization of children and parental beliefs about measles. As you go through the session you will see that many of the issues are related to management functions and the final section asks you to consider the case study in this light.
Learning Outcomes for Study Session 16
When you have studied this session, you should be able to:
16.1 Define and use correctly all of the key words printed in bold. (SAQ 16.1)
16.2 Discuss the pros and cons of a Health Extension Practitioner being local to the area where she works. (SAQ 16.2)
16.3 Describe some of the ethical issues that Health Extension Practitioners might face if they are deployed to work in their own community. (SAQ 16.3)
16.4 Explain the features of a community survey and a KAP survey as contributions to an effective health education campaign. (SAQ 16.4)
16.5 Identify some of the management issues that are part of the work of Health Extension Practitioners in relation to community surveys. (SAQ 16.5)
To reinforce your learning, this study session has several bold terms that have been defined in previous sessions of this Module. Look back to the earlier sessions if you need to remind yourself of the definitions.
16.1 Setting the scene for Alemitu’s case study
Alemitu was born and grew up in a kebele in a rural part of Ethiopia. She was a good school student and had always been interested in doing some sort of health work when she grew up. After completion of her secondary study, Grade 10, she noticed an announcement for training of Health Extension Workers. These workers would be trained at the Technical and Vocational School in her area and then deployed back to their local kebele. Alemitu was very keen to do this training and was thrilled when she was given a place as a trainee.
After one year of training, which included theoretical knowledge and skills she obtained in the classroom and practical skills sessions in health centres and a hospital in her district, Alemitu graduated as a Health Extension Worker. She was delighted when she was assigned to the Health Post in her home kebele as her first work area. Let’s pause here for a moment. Clearly being local to the area is likely to affect Alemitu’s role, but in what ways?
What do you think are the advantages and disadvantages for healthworkers when they work in their own community (like Alemitu), instead of in an unfamiliar community? Make a list of the possible advantages and disadvantages.
There are many obvious advantages to healthworkers like Alemitu working in their own community after they have been trained. They will know the local area and how difficult it is (or not) for people to access health facilities. They will know a lot about the social and cultural issues in their locality and of course be aware of the most serious health problems (Figure 16.1). They will also already know who the village leaders are and understand how decisions are made at community level. On the other hand, healthworkers who have grown up in the village in which they work will have to be especially respectful about issues such as confidentiality and privacy, because they already know a lot of personal details on the lives of community members. Alemitu will have to ensure that she works in a way that is ethical and equitable to all community members – including members of her own family. Alemitu will be known for roles other than a Health Extension Worker (for example a daughter, sister, school friend and so on). Some people may find this knowledge of her other roles quite hard to deal with.
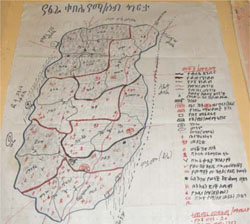 Figure 16.1 Knowing the geography, culture and people in the community in which you work is helpful in being able to provide effective health education and other health services. (Photo: Basiro Davey)
Figure 16.1 Knowing the geography, culture and people in the community in which you work is helpful in being able to provide effective health education and other health services. (Photo: Basiro Davey)
16.2 Collecting data for the community profile
Alemitu knew that the first thing she needed to do when she started her job was to collect baseline data in order to produce a community profile. So she began planning a community survey to collect data to build up the information for her community profile. She started documenting relevant facts from her previous knowledge as a member of the community, but the area was too large for her to survey every household in a short time. First, she sought the support of the kebele leaders, liaising with them and asking about their knowledge of the community and its people. This helped her to recruit community volunteers. She briefed the volunteers on how to conduct the community survey, using a specially prepared questionnaire. After training in their roles and responsibilities, Alemitu coordinated the community volunteers going from house to house asking the questions in the community survey and collecting the answers (Figure 16.2).

Some of the results of the community survey related to the geographical and social features of Alemitu’s kebele. She was able to establish that:
- The population of her kebele is 5,456 individuals, with (on average) five people per household.
- Enset or kocho is the staple diet.
- Almost all of the families within the kebele earn a living from farming.
- Many areas of the kebele are hard to reach because of the mountainous landscape.
- There is only one available dry weather road from the woreda Health Office leading to her kebele.
- Some parts of the kebele are drought-prone, so there are seasonal nutritional problems among the children.
- It takes an average of eight hours for members of her community to get to the nearest health centre.
- No local or international NGOs are operating in the kebele.
- There is limited electricity and no mobile phone access in the kebele.
- There is a traditional health delivery system offered by certain members of the community (for example, spiritual healers and suppliers of herbal medicines).
In addition to the points listed above, Alemitu needed other survey information to complete her community profile. She needed to collect demographic data on the ages, genders and circumstances of the people in every household in the kebele, whether the children and mothers have been immunized, how many women are pregnant, etc. (Figure 16.3). She also needed epidemiological data about the public health issues that affect the community, e.g. ‘Is malaria endemic in the area?’, ‘Have children died from diarrhoeal diseases or pneumonia?’, ‘What was the maternal mortality rate during the previous years?’, etc.

16.3 Collecting epidemiological data and taking appropriate actions
Alemitu was aware that she needed to add to the health data that she and the volunteers had collected from households in the community, so the next stage was to organise the remaining data collection. She obtained local records, reports and guidelines from the woreda Health Office and held discussions with her supervisor and the kebele’s community leaders. This created a mix of qualitative and quantitative data.
Look at the list below. Which of these types of data are qualitative and which are quantitative?
- Health centre and Health Post attendance figures.
- Data collected during discussion with local healthworkers about the most common health problems in the community.
- Data collected during a focus group discussion with community leaders who were asked about the priority health issues.
- Data from questionnaires on the number of cases of particular health problems in the community.
Numerical data (e.g. health centre and Health Post attendance records, and numbers of cases of particular health problems) are quantitative data. Gathering the experience and opinions of local healthworkers and community leaders adds qualitative data. Note that data gathered from questionnaires can be either quantitative or qualitative – it just depends on the questions that have been asked. For example, asking how many children someone has is a quantitative question, while asking them about their health priorities is a qualitative question (Figure 16.4).

After analysing all of the data, Alemitu identified the major public health problems of her kebele as being:
- diarrhoeal diseases
- parasites of the intestine
- respiratory problems: mainly pneumonia, but also some cases of pulmonary tuberculosis (PTB)
- malnutrition, including vitamin deficiency
- malaria
- measles among unvaccinated children.
She found that malaria, measles, outbreaks of diarrhoeal diseases and respiratory problems were among the leading causes of illness and death among children under the age of five years.
Let’s just consider again Alemitu’s place in the community.
When Alemitu has collected all the community survey data, do you think that there is a possible risk that she would be biased in prioritising her actions to resolve health problems, simply because she is a well-known member of the community?
Alemitu needed to be sure that she remained professional and as objective as possible when she reviewed and analysed the data that she collected, and decided on appropriate actions; for example, she should not try to make a particular health problem a priority for action simply because it has affected her own family. In other words, she needed to be fair and act equitably at all times.
In addition to acting equitably, what other ethical principles did Alemitu need to observe in the health services she provides? What other things did she need to bear in mind in her actions in the community?
She needed to remember the principles of beneficence and nonmaleficence. This means working in a way that ‘does good’ for the entire community, and also ensuring that actions ‘do no harm’.
16.4 Using community survey data to improve immunization coverage
After analysing the survey data collected in the kebele, and from the nearest health centre and the woreda Health Office, one of the things that Alemitu was able to establish was the immunization status of the children who were under the age of one year. She needed to know this in order to plan her immunization programmes. And, of course, therefore she also needed to know what the actual numbers were.
Look back at Figure 16.3. How many children were aged under one year in the ‘real life’ kebele pictured in that poster? What percentage of the total population were under one year?
There were 88 children aged under one year, representing 3.3% of the total population of 2,667 individuals.
Alemitu’s kebele contained 5,456 individuals. If 3.3% of community members are aged under one year, how many would you expect to find in Alemitu’s kebele?
Three point three per cent (3.3) of 5,456 is 3.3 x 5,456 ÷ 100 = 180. So you would expect to find around 180 infants under one year in a kebele of 5,456 people.
When Alemitu analysed the results of her community survey, she found that the immunization coverage of the kebele was below the national target; only 84% of the infants were fully immunized by the age of 12 months. This immediately alerted her to the need to improve the immunization coverage rates, so she began to think of ways that she could do this. One strategy was to put a chart on the wall of the Health Post to show parents how many children were not fully immunized, in order to encourage them to bring their children for vaccination (Figure 16.5). She also made plans for community conversations about the importance of immunization and asked her supervisor about increasing the number of outreach immunization visits. Notice here that Alemitu was moving forward on more than one front.
Fully immunized infants in Ethiopia have received all scheduled doses of BCG, pentavalent, oral polio and measles vaccines. In the near future, they will also receive rotavirus and pneumococcal vaccines (see the Immunization Module).

Immunization coverage is just one example of how a careful analysis of community survey data can indicate which aspects of the community health service are already doing well, and which need to be improved. After discussion with the kebele leaders and other opinion leaders in the community, Alemitu decided that the immunization problem that was most important to tackle first was the low uptake of measles vaccine. This was leading to high levels of preventable measles among children in the community. However, in order to do something about this, Alemitu needed to recognise that people had different views on the vaccine. Although some of these views might not be supported by evidence, nevertheless people would be committed to them and she needed to respect them. She also needed to acknowledge that, as with all medical treatment, things can occasionally go wrong. So you can see that there is an ethical aspect to this.
Can you think of any ethical issues that might arise during an immunization campaign?
There were several ethical issues that Alemitu had to be aware of. For example, each person has to give their informed consent to every intervention that is carried out on them or their children. This includes immunization (Figure 16.6). So Alemitu needed to ensure truthfulness in her work so that everyone knew the positive benefits of immunization, but also the small risk of an adverse reaction and what to do if it occurs.

Each person or parent has the autonomy to decide whether to accept immunization – Alemitu could not force parents to accept the measles vaccine for their children, but she had a responsibility to give them clear information to help them make a decision.
16.5 Dealing with a measles outbreak
Alemitu found several suspected measles cases among children in her kebele and reported them to the woreda Health Office. The woreda officials sent a team to investigate and confirmed the measles cases in the kebele. In the process, the team came to identify the following facts, based on the information collected from parents:
- Most of the cases were coming to the Health Post at a late stage, when some children had already developed complications of measles (pneumonia and sight problems, including blindness in one case).
- Most of the cases lived in the remote hard-to-reach areas of the kebele.
- All the cases were in children who had not been immunized with measles vaccine.
- There was a lack of awareness among community members about the importance of seeking early treatment for cases of measles.
- There were problems associated with vaccine storage and cold chain management due to a faulty refrigerator at the Health Post.
- There were problems for Alemitu in collecting and transporting new stocks of vaccine from the health centre, which was eight hours walk away from the Health Post.
Health Extension Practitioners are expected to be managers when health issues need to be sorted out in their communities. They have to take on a number of roles in order to complete their tasks. You will remember that interpersonal, informational and decisional roles are all part of what managers do in this instance. For example
- Alemitu has herself and her ability to communicate and ‘read’ situations as a resource to help her manage her relationships in the kebele.
- Being able to manage information is key both in terms of educating people and in terms of being well-informed about the actual facts of health situations (the measles outbreak in this case).
- Someone trustworthy and well-informed must take a lead in taking decisions and Alemitu in her role as a Health Extension Worker needs to be professional in doing this.
Why were these aspects of management important for Alemitu to perform when dealing with this measles outbreak?
The interpersonal role was important because so many people needed to be involved; Alemitu had to communicate with them all, so they knew what they were expected to do. The informational role is also important because each person who is in the team needed to have the correct information about the measles outbreak. The decisional role is important as well – people look to the Health Extension Practitioner to take decisions about the way to tackle health issues in their community.
As part of the response to the measles outbreak, the woreda team recommended a rapid assessment of the knowledge, attitude and health practices (KAP) of the community on measles management at kebele level. The woreda supported Alemitu in collecting data in a KAP survey. They identified elders, religious leaders and traditional health service providers, as well as parents, as particularly informative subjects to study. They collected data after developing interview questions for individuals and groups. Privacy and confidentiality are key ethical considerations in interviewing people on sensitive topics.
How do you think Alemitu should deal with privacy and confidentiality when interviewing for a KAP survey?
Alemitu would have to be aware of privacy issues and conduct sensitive interviews in a place where nobody else could overhear the conversation. Confidentiality is also important: she must not talk about the details of any sensitive matters that her interviewees had told her. If she took notes during the interviews she should be sure that nobody else could read them not only by keeping them in a safe place but also handling them in such a way that no one could ‘look over her shoulder’ and see what the last interviewee said.
The KAP study resulted in the following findings:
- The community was aware of the symptoms of measles and they had a local word for the illness.
- They believed that a child with measles has to stay at home in a quiet environment, not exposed to sun, and must not cross the river.
- Measles was thought to be a self-limiting disease by the community (i.e. children would recover naturally); therefore parents of children with measles need not seek treatment from the formal health service.
- There was a widespread belief that giving an injection to a child with measles would kill the child.
The woreda health officials and Alemitu planned a health education programme (Figure 16.7) targeting the mistaken beliefs identified in the above findings. Particular individuals and groups were identified as the main target for the health education programme. Alemitu identified schools, churches and mosques, community meeting places, kebele meetings, the Health Post and the health centre as suitable settings for health education to take place. The key health education messages were identified to convince the community members that measles is a very serious illness, which can kill a child, or permanently damage its sight and cause severe respiratory problems. A child with measles should be taken to the Health Post or Health Centre for urgent treatment for these complications. Children can be protected from measles by immunization with a single injection of a safe vaccine at nine months of age.

Alemitu’s plan included a strategy for monitoring these interventions to assess whether they resulted in changed behaviour concerning measles treatment and immunization. One way in which the monitoring was carried out was to count the number of people (community members, religious leaders, traditional healers, etc.) who attended each of the health education events. Afterwards, Alemitu and the woreda health officials checked to see how many of the unvaccinated children were brought for measles immunization by parents who attended the meetings, or who heard the messages from their neighbours, community leaders and other influential people. They also interviewed community members to ask if their knowledge, attitudes and practices had been changed by hearing the health messages in the campaign.
The results of the evaluation were good. The campaigns under Alemitu’s leadership were shown to be very effective. Within two years the measles immunization coverage in the kebele was found to have increased to 96%. There were only five cases of measles among unvaccinated children and all the parents quickly brought the sick child for treatment. Through her work Alemitu set up control of the project by establishing what was going on at the beginning and working through to establish how things had improved. For the success she achieved in her work, the community members and woreda Health Office recognised Alemitu as a ‘Change Agent’ in her community.
Now you have read about Alemitu’s work on immunization and the measles outbreak, you can see how she has been engaged in health management. You will remember from Study Session 2 that the key functions of management are: planning, organising, leading, coordination, monitoring and control. You will recall too that interpersonal, informational and decisional activities are required of someone undertaking a management role.
Look back through this extended case study and note the places where these key management functions are mentioned (they have been highlighted in bold). Briefly describe how Alemitu undertook these tasks as part of her role as a Health Extension Worker.
Alemitu started her job by planning a community survey to collect the baseline data she would need for her community profile. She liaised with key people in the community in order to select volunteers. She then trained the volunteers and organised and coordinated the process of collecting survey data. Alemitu maintained control by monitoring the outcomes of the interventions to check that the objectives were achieved. Throughout this process, Alemitu demonstrated her leadership skills at all stages.
Summary of Study Session 16
In this extended case study, you have learned that:
- Creating a community profile is one of the first tasks that is expected of a Health Extension Worker or Health Extension Practitioner.
- A good community profile will contain social and economic features that will help the healthworkers understand who is in the community.
- Community profiles also contain health data that will show what illnesses are the most important in the community.
- Data for the community profile can be collected by the healthworkers or by specially trained volunteers going from house to house.
- Health data can be collected from official sources and may be either quantitative or qualitative, or a mixture of both types of data.
- The data collected by a number of methods will establish the most important diseases to be tackled in the community.
- A detailed plan of implementation will be required to tackle the health problems that have been identified.
- Monitoring of the execution of campaigns is important to examine their success, and the control of knowing how much has changed is important too.
- Management is an integral part of the role of a Health Extension Worker.
Self-Assessment Questions (SAQs) for Study Session 16
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Some of the questions address Learning Outcomes from previous study sessions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 16.1 (tests Learning Outcomes 16.1)
Match the following objectives with the descriptions below.
Two lists follow, match one item from the first with one item from the second. Each item can only be matched once. There are 7 items in each list.
Geographical
Social
Demographic
Epidemiological
Qualitative
Ethical
Quantatitive
Match each of the previous list items with an item from the following list:
a.Data about hard facts and numbers.
b.Knowing how long it takes people to reach healthcare facilities.
c.Data about public health issues, for example the incidence of measles in a community.
d.Data about gender and age.
e.Data about people’s understanding and beliefs.
f.Being aware of how a local community works, for instance in its decision making processes.
g.Behaving in a good way and doing no harm; behaving with moral integrity.
- 1 = b,
- 2 = f,
- 3 = d,
- 4 = c,
- 5 = e,
- 6 = g,
- 7 = a
You will be familiar with most of these key words. However in this session they appear in a very practical case study so just check carefully that you can see how they are used in this applied sense.
SAQ 16.2 (tests Learning Outcome 16.2)
Divide the following list into two separate lists, In List A, note ways in which the fact that Alemitu is local may help her in her role as a Health Extension Worker and in List B, note the ways in which being local might possibly create problems.
- She knows the local geography.
- She is known for other personal roles as well as being a Health Extension Worker.
- She is well aware of the social and cultural issues of the community.
- People possibly may think she is biased towards the interests of her own family.
- People may have concerns about privacy and confidentiality because she knows the people very well.
- She understands how community decisions are taken.
- She knows who the leaders and key people in the community are.
Answer
List A = 1, 3, 6, 7.
List B = 2, 4, 5.
Remember though that although the issues in List B need thinking about carefully, there is no reason why Alemitu as a professional Health Extension Worker cannot deal with them.
SAQ 16.3 (tests Learning Outcome 16.3)
Look at the list below. Put an A next to any issues that are about something other than ethics for a Health Extension Worker.
Put a B next to any issues that you consider to be unethical. (Some of the points will appear on neither list!)
- Being truthful to parents about any risks associated with the measles vaccine.
- Being careful about respecting the privacy of people being interviewed.
- Working out the number of children under one year old who have not been vaccinated.
- Vaccinating children without getting informed consent.
- Telling friends and relatives about what people have said in interviews.
- Working out how long to spend on the community survey.
Answer
You should have A next to 3 and 6, and B next to 4 and 5.
1 and 2 are part of the ethical concerns of a Health Extension Worker (or Practitioner) and so should appear in neither list. 3 and 6 are practical not ethical issues. 4 and 5 are unethical. A Health Extension Worker should always seek informed consent, which means people have the right to know the full facts and then make their minds up whether to go ahead. Health Extension Worker’s need to value privacy and confidentiality at all times. This respects people but also it makes a Health Extension Worker a figure of trust in the community.
SAQ 16.4 (tests Learning Outcome 16.4)
What is the difference between a community survey and a KAP survey?
Answer
A community survey is mostly about facts and figures, about how many people there are and their ages, gender, occupation, etc. It is also about people’s access to health facilities.
A KAP survey is more about people’s understanding, beliefs, attitudes and knowledge of health in the community they live. You need to know what your community thinks and believes.
Both sorts of surveys are vital in planning campaigns. You need to know the facts and figures and you also need to know what people think.
SAQ 16.5 (tests Learning Outcome 16.5)
Match the following management functions with the descriptions below.
Two lists follow, match one item from the first with one item from the second. Each item can only be matched once. There are 6 items in each list.
Planning
Organising
Coordinating
Leading
Monitoring
Control
Match each of the previous list items with an item from the following list:
a.Taking the responsibility for the project and being at the forefront to take people forward.
b.Setting up an aspect of the project so you are sure how behaviour has changed and how much it has changed.
c.Making sure that different aspects of the overall project fit together, including people working, timings and so on.
d.Determining a course of action through careful estimation of the situation now and where you want to get to.
e.Enabling the project through effective deployment of people and documents so everyone knows what they are doing.
f.Checking progress on the project to see whether it leads to changed behaviour.
- 1 = d,
- 2 = e,
- 3 = c,
- 4 = a,
- 5 = f,
- 6 = b
Management is a complex process and the functions we have outlined do not always fall into a simple order. For example, sometimes you will plan several times during a project and set up several small targets at different stages. You will also need to assess if you have achieved those targets. Plans come in all shapes and sizes from the planning of the overall project through to who is going to interview whom this morning. It is a matter of being aware all the time of the stage you have reached and which function is appropriate at ‘this stage’ in the project.