Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Thursday, 12 February 2026, 6:26 PM
Non-Communicable Diseases, Emergency Care and Mental Health Module: 14. Substance Use Problems
Study Session 14 Substance Use Problems
Introduction
In this study session, we use the term ‘substance’ to mean any drug, both legal (e.g. alcohol, tobacco) and illegal (e.g. cannabis) that can cause dependence.
Throughout history human beings have used substances to alter their state of mind. Substances can alter thoughts, emotions, sleep, appetite and social interactions. They are also used to relieve pain and tension. There are a wide range of substances used, and the number of people using substances has increased alarmingly in recent years. In many countries, including Ethiopia, substance-related problems are a major public health concern. It is important that steps are taken at the community level to prevent the increasing problem of substance use.
In this session you will learn about commonly used substances in Ethiopia, their effects, early recognition, referral and treatment, and what can be done to prevent people using substances.
Learning Outcomes for Study Session 14
When you have studied this session, you should be able to:
14.1 Define and use correctly all of the key words printed in bold. (SAQ 14.1)
14.2 Describe the immediate and long-term effects of alcohol and other substances that are abused. (SAQ 14.2)
14.3 Explain how to correctly use a screening tool to identify harmful use of alcohol. (SAQ 14.3)
14.4 Describe how to manage people with substance use problems at the community level. (SAQ 14.4)
14.5 Explain the reasons for referring people with substance use problems and where to refer them. (SAQ 14.4)
14.1 Substance use problems
In this section we will define commonly used terminology in connection with substance use and abuse. We will also discuss the process of substance use initiation and how this can develop into addiction.
Psychoactive substances are substances which, when taken into the body, have a major effect on the brain and can alter physical and psychological functioning. Many people enjoy the psychological changes in mood and thoughts that psychoactive substances can bring about. As a result, people often develop a habit of taking the drugs more frequently. These substances are therefore also referred to as habit-forming substances.
14.1.1 Why do people initiate substance use?
There are many reasons why people start to use and continue to use substances. The substances may be taken to reduce stress and alleviate pain, or alternatively to stay alert, to stimulate the mind in order to study or to better perform some task, or simply to have fun with friends. People with mental health problems may take substances to ‘treat’ symptoms (although you should recall from Study Session 13 that this is very unwise because it can aggravate symptoms and limit the effectiveness of antipsychotic medication).
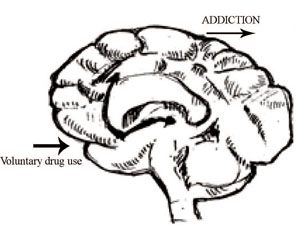
Some disadvantaged members of the community (for example, people who are unemployed or youth out of school) may use substances to occupy their time. Young people often initiate drug use out of curiosity or because of peer pressure. You may be wondering why people continue to use substances. After repeated drug use, ‘deciding’ to use substances is no longer voluntary because the substances induce changes in brain function, which leads to addiction (Figure 14.1).
14.1.2 How substances affect the brain
Substances interact with the brain and affect its function in many ways. For example, by changing a person’s mental processes and behaviour, substances can affect memory, attention and the way people talk. They can also increase impulsiveness, which can lead to aggression and violence. You may also notice changes in the level of alertness and perception of the world.
Addiction (also called dependence) is a complex illness characterised by compulsive behaviour (the person has a compelling need to use a substance), and uncontrollable cravings (having a strong desire to get the substance). People who are addicted to psychoactive substances persist in using the drug even in the face of extremely negative consequences (e.g. family or job problems, being jailed).
People with addiction typically need increasingly high doses of the drug to achieve the same effect (this is called tolerance), and when they try to stop or reduce the intake of the drug they develop adverse physical and/or psychological symptoms, called withdrawal effects.
Substance abuse is frequent use of a substance despite negative consequences. Not all drug use is bad. Many people have the occasional glass of alcohol and don’t develop any negative effects. It is only when someone shows harmful use of substance (e.g. excessive drinking that is damaging to physical and mental health) that problems develop.
From you own observation, what kinds of substances do you think are commonly abused in Ethiopia?
Alcohol, cigarettes, khat and cannabis are all drugs that frequently lead to addiction in Ethiopia.
Habit-forming substances can be divided into different classes according to their effect (Figure 14.2).
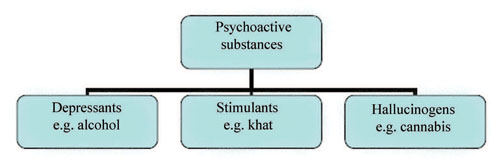
Depressants are substances that have a relaxing effect on people by reducing the activity in the brain. Examples of depressants include alcohol and drugs prescribed for sleep problems.
Stimulants are substances stimulating the brain, e.g. khat and tobacco.
Hallucinogens are substances producing hallucinations, e.g. cannabis may produce hallucinations if taken in large amounts.
14.2 Alcohol use
Alcohol is a habit-forming substance that is present in varying amounts in beer, wine, and spirits. Examples of Ethiopian local drinks that contain alcohol are tella, tej, and areki (Figure 14.3).

Moderate use of alcohol does not have major consequences for health; the substance use becomes problematic when someone uses a lot of alcohol, and/or consumes alcohol throughout the day, especially in the morning. Box 14.1 sets out the guidelines for healthy alcohol use. In addition to these guidelines, a person who drinks in the morning may well have health and social problems related to alcohol consumption.
Box 14.1 Maximum alcohol limits a person can drink
For men = 21 units per week (or on average three units per day)
For women = 14 units per week (or on average two units per day)
(1 standard unit = 6–8 grams of alcohol: a shot of spirit or areki contains approximately 1 unit of alcohol, a bottle of beer contains about 1.5 units and a glass of wine about 2 units.)
What is the recommended daily limit of beer intake for men?
Men are advised not to drink more than two bottles of beer (or three alcohol units) on average per day.
14.2.1 Immediate effects of alcohol use
The immediate effects of alcoholic drinks are seen soon after drinking excess amounts of alcohol. A typical effect on mental status is sedation (it makes people sleepy). There are also other effects on the body, e.g. a lower heart and respiration rate, a slower reaction time (speed of reaction of a person to an incident requiring a fast response), impaired coordination (e.g. difficulty in walking straight), and even loss of consciousness in the case of very heavy alcohol intake.
14.2.2 Long-term complications of alcohol use
The long-term effects of alcohol are seen after drinking alcohol for years. Alcohol affects most organs of the body including the brain. Long-term heavy alcohol use can lead to brain damage, which may in turn lead to loss of memory. People with alcohol abuse may, for instance, forget familiar places (e.g. they walk aimlessly, often missing their own houses) or may no longer recognise people who are familiar to them. The brain damage may also cause slurred speech and decreased motor coordination. Alcohol abuse can also lead to deficiencies in nutrition. People with alcohol problems often eat poorly (limiting their supply of essential nutrients) and alcohol interferes with the nutritional process in the body, so that the nutrients are not fully absorbed. Alcohol may also affect the fetus if a pregnant woman consumes alcohol. The use of alcohol increases the risk of delivering a low birth weight baby and may increase the child’s risk of developing learning difficulties later in life.
14.2.3 Withdrawal effects of alcohol use
Withdrawal effects of alcohol use can occur when people with alcohol use problems suddenly decrease or stop using alcohol. The majority of people with alcohol use problems have mild to moderate withdrawal symptoms, including tremors (shaking hands), sweating, sleep disturbance, decreased appetite and nausea. These withdrawal symptoms usually disappear in less than seven days with or without treatment. Sometimes the withdrawal symptoms can be very severe, and lead to an emergency medical condition called delirium tremens. Delirium tremens is characterised by loss of consciousness, agitation, restlessness, tremor, disorientation (difficulty in knowing place and time or recognising familiar people), sweating and high fever, visual hallucinations, and paranoia. It commonly occurs three to seven days after drinking has stopped.
14.2.4 Identification of people with drinking problems
The best way of identifying people with alcohol use problems in your community is to ask routinely about drug and alcohol use. The questions in Box 14.2 come from a screening questionnaire called CAGE. These questions will help you to identify people with alcohol use problems.
Box 14.2 Identifying someone with a drinking problem
Questions to ask the family or friends:
- Has the person been drinking recently?
- Are your worried about his or her drinking? Why?
- Has the person been drinking in the mornings?
Screening questions to ask the person (CAGE questionnaire):
- Have you ever felt you should Cut your drinking?
- Have people Annoyed you by criticising your drinking?
- Have you ever felt bad or Guilty about your drinking?
- Have you ever taken a drink first thing in the morning (Eye opener) to steady your nerves or get rid of a hangover?
Yes to two or more questions suggests the person has a harmful drinking problem.
Whilst you talk to the person, look out for signs of tension, nervousness, the smell of alcohol, bruises, scars or other signs of injuries. When these signs are present it is possible that this person is suffering from alcohol-related problems. After identifying the person with alcohol-related problem, the next step is to help them solve the problem.
14.2.5 Management of people with alcohol-related problems
The goal of treatment is to help the individual live a normal life without alcohol use. This would include the acute phase of withdrawal when medical help is needed and the longer phase of readjustment to normal life and rehabilitation.
The first step is to help the individual and family to accept the problem. In the process, it is important that you understand the patient’s perspective and attitude towards drinking. Successful treatment depends on the attitude and confidence of the patient. For patients willing to stop, advise them to set a definite date to quit. The preferred goal of treatment should be abstinence. However, abrupt abstinence for a person with a heavy alcohol drinking habit may lead to severe withdrawal symptoms (as described above).
When you deal with people with alcohol problems, you should explain the benefits of reducing or stopping drinking alcohol to them. Stopping using alcohol can save them money, reduce the risk of liver disease, depression, weight loss, brain damage, sleep disturbances and accidents. There is also the benefit of reducing problems at work with their employer or workmates, reducing criticism and insults from the family, and avoiding legal problems (e.g. being arrested for fighting and other criminal acts while under the influence of alcohol).
The second step for your client is to seek assistance from the nearest health facility. Advise the patient and refer them for medical treatment at the health centre or nearest hospital.
Why should a person withdraw from alcohol under medical supervision in a health facility? Think about what you have read in Section 14.2.3.
Sudden withdrawal can result in severe symptoms, including delirium tremens. Such patients should be referred because medical supervision is important.
14.2.6 When you should refer a person
You should refer the person if they are drinking large amounts of alcohol or have developed a severe withdrawal reaction, or when there is a serious medical condition like diabetes mellitus, or chronic liver disease. If a person has a severe mental illness (SMI, see also Study Session 10) in addition to their alcohol use, then they should be referred to the nearest mental health service. When the person is taking multiple substances, in addition to alcohol, they should be referred to the nearest substance treatment centre or mental health centre with an in-patient service.
14.2.7 Other advice you can give your local community
Apart from your role in identifying individuals with alcohol-related problems in your community and managing their problems, you can play an important role in educating people about the effects of alcohol. Box 14.3 lists some ways in which you can be of help.
Box 14.3 How can you help to reduce alcohol use problems?
As a locally trusted healthworker you can help to reduce alcohol use problems in your community in the following ways:
- By being available and helping people with alcohol use problems to accommodate to changes in their lifestyle.
- Educating people about the immediate and long-term adverse effects of alcohol use.
- Giving information to patients and their families that alcohol dependence is an illness with serious consequences.
- Mothers should be advised against drinking during pregnancy because drinking may harm the fetus.
- People with physical diseases and/or dependency should be recommended to abstain from taking alcohol.
14.3 Tobacco use problems
Tobacco products contain the chemical compound nicotine, which is addictive. Other components in tobacco, especially tar, affect the respiratory system and increase the risk of lung cancer and other chronic respiratory problems. People in the rural community of Ethiopia use tobacco through smoking, chewing and putting a bolus of tobacco under the tongue.
Globally about one in three adults smokes i.e. 1.2 billion people. By 2025 the number is expected to rise to more than 1.6 billion, so smoking is clearly a worldwide problem.

14.3.1 Immediate effects of tobacco use
The popularity of tobacco mainly stems from its immediate effects which – users state — include feeling happy and relaxed and improved concentration. However, evidence suggests that smokers are actually less able to be happy or relaxed or concentrate than non-smokers when they do not have access to tobacco (see Section 14.3.3). The immediate physical effects of smoking tobacco include increased blood pressure, respiration and heart rate. With regular tobacco use, levels of nicotine accumulate in the body during the day and persist overnight. Thus, daily smokers or chewers are exposed to the effects of nicotine for 24 hours a day. Nicotine stimulates the brain (see Section 14.1). Stimulation is then followed by depression and fatigue, leading the user to seek more nicotine.
14.3.2 Long-term effects of tobacco use
Long-term use of tobacco can lead to a wide range of health problems including cataracts of the eye (see Study Session 5) and greatly increases the risk of cardiovascular and respiratory diseases including lung cancer (see Study Session 3). Smoking during pregnancy is especially harmful as it may result in delivery of a low birth weight baby, which in turn is a risk factor for later mental and physical problems in the child. Passive smoking (when somebody is exposed to smoke through the smoking of someone else) can also cause lung cancer in adults and increases the risk of respiratory illnesses in children and sudden death in infants.
14.3.3 Withdrawal effects of tobacco
Research has found that when chronic smokers are deprived of cigarettes for 24 hours, they display increased levels of anger, hostility and aggression, and are less inclined towards social cooperation. Tobacco users suffering from withdrawal also take longer to regain emotional equilibrium following a stressful experience. During periods of abstinence and/or craving, smokers tend to show decreased motor activity and concentration, and loss of interest in work.
14.4 Khat abuse
Khat is an evergreen shrub grown in east Africa and used as a stimulant. Khat contains more than 40 chemicals. Most of the stimulant effect of khat is thought to come from the chemicals cathinone and cathine. Khat can be chewed, or may be brewed as tea. It can also be swallowed with a soft drink. The prevalence of khat use in different parts of Ethiopia is variable ranging between 0.3% and 64%. People usually prefer to chew khat in groups (Figure 14.4).

14.4.1 Immediate effects of khat use
People chew khat because they believe that, like tobacco, it improves their concentration. During and immediately after chewing khat, people state they feel euphoric and wakeful, and have increased energy. They are also likely to have a decreased appetite (and are consequently often underweight) and an increased body temperature. Khat can also provoke paranoia and aggressiveness.
14.4.2 Long-term effects of khat use
People who have used khat for more than a few years may manifest with a range of serious symptoms (see Figure 14.5), including depression, anxiety, irritability, anger, sleep disturbance, fatigue, suspiciousness, hallucinations, panic attacks, suicidal thoughts, dry mouth, burned lips, worn teeth, disturbances in heart rhythm, heart attack and loss of libido.

14.4.3 Withdrawal effects of khat use
The withdrawal effects of khat use are usually seen in people who have been using khat for long time. These are especially visible during early afternoons when many people chew khat:
- Sadness
- Loss of interest in work and social interaction
- Reduced activity
- Vivid unpleasant dreams, popularly called dukak in Ethiopia.
14.5 Cannabis (hashish or marijuana)

Cannabis is a dry, shredded green/brown mix of flowers, stems, seeds and leaves of the plant Cannabis sativa. It has many informal names (e.g. ‘ganja’, ‘weed’, ‘torpedo’, ‘dope’) and is usually smoked as a cigarette (Figure 14.6), but it can also be eaten. Marijuana smoke has a distinctive sweet smell. The active ingredient in cannabis is called delta-9-tetrahydrocannabionol (THC). THC has a direct effect on the brain.
14.5.1 Immediate effects of cannabis
Cannabis is rapidly absorbed and metabolised when smoked, less so when ingested (although this can produce a more intense effect). The immediate effects include a sense of relaxation, increased appetite, mood change, reduced thinking capacity, suspicion and paranoia, and impairment in balance. Cannabis may also cause hallucinations, delusions, agitation and panicky feelings in vulnerable individuals. If you observe a person during or immediately after smoking, you may notice the strong smell, and the smoker may have red eyes and a flushed face.
14.5.2 Long-term effects of cannabis
Long-term frequent cannabis use leads to lack of motivation and poor performance at work or in school compared to individuals who do not consume this drug. People with cannabis use problems often appear tired and seem to not care about what happens in their life, have no desire to work regularly, and have a lack of concern about the way they look. In people who have a genetic vulnerability to psychosis, using high doses of cannabis for a prolonged period may act as a trigger to induce psychotic episodes (see Study Session 13).
14.5.3 Withdrawal symptoms of cannabis
Withdrawal from cannabis can provoke a range of both physical and psychological symptoms. These include interrupted sleep or — in extreme cases — total insomnia. When long-term heavy users of cannabis reduce or stop taking the substance, they may lose interest in eating and experience nausea and diarrhoea. They may also become irritable and restless and sweat excessively.
14.6 Identification of people with tobacco, khat or cannabis use problems
If you see a person with poor physical health or who is prone to repeated accidents, or has a reputation for failing to live up to their responsibilities, ask if they use any of the substances mentioned above. Ask the questions in Box 14.4 to help you to identify and help people with tobacco, khat or cannabis use problems.
Box14.4 Identifying someone with a tobacco, khat or cannabis use problem.
Questions to ask family and friends:
- Have you noticed any change in their behaviour or that of their friends? If yes, what is the nature of this behaviour and when did it start?
- Do you suspect they are chewing khat, smoking cigarettes or using cannabis?
- How do you feel about this? (This question is helpful because the attitude of the family towards substance abuse is an important factor in treatment, especially in developing countries such as Ethiopia.)
Questions to ask the person using tobacco, khat or cannabis:
- Have you been chewing khat or smoking cigarettes and/or cannabis?
- In what situations do you chew khat or smoke cigarettes and/or cannabis?
- How is the use of khat, cigarettes or cannabis affecting your health? Your family? Your work?
- Have ever you tried to stop chewing khat, or to stop smoking cigarettes or cannabis on your own?
- Would you like to stop using khat, cigarettes and/or cannabis?
- Who is supporting you now? (This question is relevant because the presence of social support is an important factor in the success of treatment.)
14.7 Management of people with cigarette, khat and cannabis use problems
The goal for treatment of people with cigarette, khat and cannabis problems is to help them live a normal life without substance use, so that they can function normally both in their daily social life and in their work. Treatment starts by assessing the degree of motivation and motivating them to pass through the process of change in their lifestyle. It involves increasing awareness; enhancing motivation, and helping them through the process of change. The next step is to seek assistance from the nearest health facility. Advise and refer the patient for further treatment at a health centre, the nearest hospital, or a substance abuse treatment centre for further evaluation and treatment.
14.7.1 When to refer for these substances
People with substance abuse problems should be referred to a health centre or general hospital when there is a serious medical condition, for example, diabetes mellitus or chronic liver disease. If the patient has a severe mental disorder, like psychosis, they should be referred to the nearest mental health service for better evaluation and management (see also Study Session 13). When people use large amounts of substances and/or multiple substances, or if they are unable to stop despite your guidance, they should be referred to a substance abuse treatment centre or to a hospital with a psychiatrist.
Summary of Study Session 14
In Study Session 14 you have learned that:
- Addiction is a condition where a person has uncontrollable drug cravings and takes the drug compulsively, despite the negative consequences associated with the substance use.
- People start using drugs for different purposes. When substances are taken frequently and excessively they may result in brain change. As a result addiction may occur and the addicts’ control of their substance use may become increasingly difficult.
- People with substance abuse problems often need increasing amounts of drugs to achieve the same effect (tolerance) and they show withdrawal symptoms after decreasing or stopping the use of the drug.
- Some of the immediate effects of popular substances are pleasurable. The drug can for instance have a relaxing effect (e.g. in the case of alcohol), or improve concentration (e.g. tobacco, khat). Long-term substance abuse, however, has serious adverse effects, including brain damage (alcohol), lung cancer (tobacco), depression and anxiety symptoms (khat) or paranoia and psychosis (cannabis).
- Alcohol, tobacco, cannabis and khat use can be identified by asking specific questions to the person and their family. People with substance abuse problems should be encouraged to stop using the drug by educating them about the negative effects and supporting them in making the necessary lifestyle changes.
- In cases of serious withdrawal symptoms, severe medical conditions or mental health problems, the person with a substance use problem should be referred to the nearest health centre for further assessment and treatment.
Self-Assessment Questions (SAQs) for Study Session 14
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering these questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 14.1 (tests Learning Outcome 14.1)
Which of the following statement is false? In each case explain why it is incorrect.
A Every psychative substance will cause dependence.
B Tolerance refers to the need to increase the amount of psychoactive substance to achieve the same effect.
C People who are addicted to alcohol and cannot stop drinking only have themselves to blame.
D The presence of withdrawal symptoms is one sign of dependence.
Answer
A is false. Psychoactive substances can cause addiction, but many people use substances, for example alcohol, in low amounts without becoming addicted.
B is true. Psychoactive substances can cause tolerance, which is characterised by the need to increase the quantity of substances used in order to get the same level of effect as before.
C is false. This person may have started using substances voluntarily, but after a certain period of time brain changes will lead to involuntary use. This means the person should receive help and support in overcoming their addiction.
D is true. People who have developed an addiction will show withdrawal symptoms. Which particular symptoms are likely to occur depends on the type of substance used.
Read Case Study 14.1 and answer the question that follows it.
Case Study 14.1 Mr Thomas
Mr Thomas is a 39-year-old merchant and a married father of two. He has been drinking local areki on a daily basis for the last 10 years. He initially took up drinking to socialise with his friends, but over time he has greatly increased the amount of areki he drinks. He feels a craving to get areki all the time. His wife is worried about his forgetfulness, his loss of interest in work, the lack of money to feed the family and the many domestic arguments they have. He exhibits irritable behaviour, tremor, sweating and nausea. His wife says he looks tense and fearful whenever he has a day without drinking areki.
SAQ 14.2 (tests Learning Outcome 14.2)
Outline the withdrawal symptoms and long-term effects impacting on Mr. Thomas of his areki drinking.
Answer
Mr Thomas’s withdrawal symptoms include: a compulsion to drink, irritable behaviour, tremors, sweating, nausea and feeling tense and fearful when deprived of drink.
Long-term effects are: forgetfulness, loss of interest in work, failure to manage family commitments and financial difficulties.
SAQ 14.3 (tests Learning Outcome 14.3 and 14.5)
After reading Case Study 14.1, what questions would you ask Mr Thomas to find out whether he has an alcohol use problem?
What would make you decide whether to refer Mr Thomas for medical treatment?
Answer
You should use the questions in the CAGE questionnaire (Box 14.2):
- Have you ever felt you should Cut your drinking?
- Have people Annoyed you by criticising your drinking?
- Have you ever felt bad or Guilty about your drinking?
- Have you ever taken a drink first thing in the morning (Eye opener) to steady your nerves or get rid of a hangover?
Based on the information provided in the Case Study, Mr Thomas seems to have developed an alcohol addiction. From the CAGE questions you ask Mr Thomas, and from talking to Mr Thomas’s wife, you can evaluate the severity of the addiction, his withdrawal symptoms and whether Mr Thomas may have other physical or mental health problems. In cases of severe withdrawal symptoms or other physical or mental health problems, you should refer Mr Thomas to the nearest healthcentre or hospital.
SAQ 14.4 (tests Learning Outcomes 14.4 and 14.5)
Mr Nuredin has been chewing khat and smoking cigarettes for more than 15 years. He comes to you and asks you ‘Is there a need to stop chewing khat and smoking cigarettes?’ How would you respond?
Answer
Mr Nuredin has been chewing khat and smoking cigarettes for 15 years. You should encourage him to stop using these substances by giving him adequate information about the negative consequences of using them. You can also support him in his efforts to stop taking the drugs by assisting and advising him in making changes to his lifestyle. You should advise him to see a doctor if he cannot stop without medical assistance.