Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Friday, 21 November 2025, 5:50 AM
Adolescent and Youth Reproductive Health Module: 8. Contraceptive Options for Young People
Study Session 8 Contraceptive Options for Young People
Introduction
The Family Planning Module covers the different methods of contraception. In this session you will learn about contraceptive options that are suitable for young people (remember that by young people we mean those aged 10–24). If a girl becomes pregnant when she is very young, it can be damaging to her physically and can also have bad social and economic consequences for her and her partner. You will help young people by counselling them on delaying pregnancy and childbearing and by providing appropriate contraceptive methods. Many young people avoid using contraceptives or discontinue using them either because they have misinformation about contraceptive methods or because they are worried by side effects. It is important to dispel misinformation about contraceptives and address the side effects of contraceptive use to ensure that young people choose a suitable method of contraception and continue to use it properly.
Learning Outcomes for Study Session 8
When you have studied this session, you should be able to:
8.1 Define and use correctly all of the key words printed in bold. (SAQs 8.1, 8.2, 8.3, 8.4 and 8.5)
8.2 Explain why it is important for young people to delay pregnancy and childbearing. (SAQ 8.1)
8.3 Identify and explain contraceptive methods appropriate for young people. (SAQs 8.2, 8.3, 8.4 and 8.5)
8.4 Review emergency contraception and its role in prevention of unwanted pregnancy. (SAQs 8.5 and 8.6)
8.1 Why it is important to delay pregnancy and childbearing
8.1.1 Health risks of early pregnancy
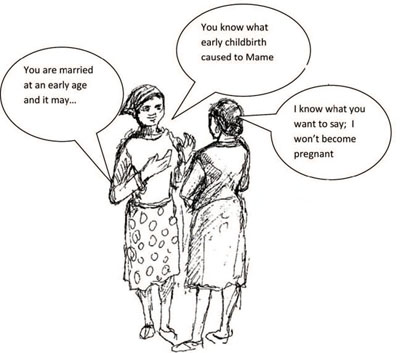
Pregnancy before the age of 18 has several health risks (Fig 8.1). Some of these health risks include:
Prolonged or obstructed labour: adolescents younger than 18 often have not reached physical maturity and when they become pregnant, their pelvises may be too narrow to accommodate the baby's head during delivery. In these cases, obstructed delivery and prolonged labour are more likely, thereby increasing the risk of haemorrhage (bleeding), infection and fistula.
Pre-eclampsia (hypertension in pregnancy) is common in adolescent pregnancy. If it is left uncontrolled, it can progress to extreme hypertension. This condition could lead to the death of both the young mother and the baby.
Premature birth and stil birth: infants born to adolescent mothers are more likely to be premature, of low birth weight, and to suffer consequences of retarded fetal growth. Stillbirth is more common among adolescent mothers than older mothers.
Pregnancy in adolescents, especially if they are unmarried, is almost always unwanted.
What do you think unwanted pregnancy could lead to in young girls?
Unwanted pregnancy in adolescents could cause them to resort to unsafe abortions. As you have seen in Study Session 4, unsafe abortion is among the common causes of maternal deaths in Ethiopia.
Stop reading for a moment and think about the following question from your experience in your community. What other consequences of early pregnancy in adolescent girls can you think of? (You can answer this by thinking about what you have learned in Study Session 3 of this Module.)
In addition to the health risks, early pregnancy has psychological, social and economic consequences for both girls and boys, some of which are presented below.
8.1.2 Psychological and other consequences of early pregnancy for girls

Some of the consequences are:
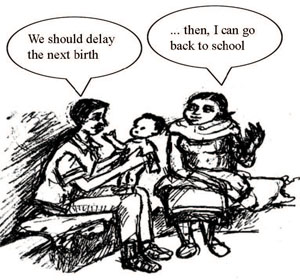
- Pregnancy often means the end of formal education for adolescents because they drop out of school when they become pregnant. (Figure 8.2)
- Adolescent pregnancy changes a girl’s choice of career, opportunities and future marriage. Mostly unmarried mothers resort to low-paying and risky jobs, domestic work, and even prostitution to support their children.
- Early marriage due to an unplanned pregnancy is frequently an unhappy, unstable one that leads to divorce. Both mother and child face the stigma of illegitimacy when marriage doesn’t take place or when divorce occurs.
- Young mothers are often ill-prepared to raise a child, which may lead to childrearing problems like child abuse or neglect.
- Girls resorting to prostitution due to early and unwanted pregnancy are at higher risk of gender-based violence, substance abuse, and STIs such as HIV.
8.1.3 Psychological and other consequences of early pregnancy for boys
Some of the consequences are:
- Some boys refuse to take responsibility for the pregnancy, which can contribute to hardship for the mother and child and also can lead to future regret.
- Boys who become fathers lose opportunities for education and future economic advancement. Those who marry leave school to support their new families.
- Young fathers are often ill-prepared to raise a child, which may lead to childrearing problems like child abuse or neglect.
- Premature marriages which occur because of early pregnancy are frequently unstable and end in divorce.
As you have seen, pregnancy in adolescence has several bad effects. For this reason, it is important to prevent pregnancy in adolescents or delay it until a couple is in a secure and loving relationship. (Figure 8.3)
What should adolescents do to prevent pregnancy?
As you have learned in the Family Planning Module, they should use contraceptives to prevent pregnancy and childbearing.
In Section 8.2 you will learn which contraceptive methods are the most appropriate ones for young people.
8.2 Contraceptive methods for young people
8.2.1 Combined oral contraceptives (COCs)
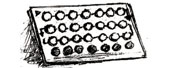
COCs are appropriate and safe for young people. Many young people choose a COC because this method has a low failure rate and also offers relief from dysmenorrhea (pain during menstruation). It is a straightforward method that does not interfere with sexual intercourse. This is a good method for you to recommend when it is clearly appropriate for the girl; the particular COC you would suggest will depend on what is available. Some pills are more oestrogen-dominant and others are more progestin-dominant. A COC with more progestin is helpful for girls who have painful and excessive menstrual bleeding.
Failure rates are higher for young girls than for older women. This is because young girls often fail to take pills regularly. Failure to take pills regularly is often due to lack of knowledge about pill taking. You should encourage condom use in addition to COCs for STI/HIV protection.
Will a COC protect the girl from sexually transmitted infections (including HIV)?
No, it offers no protection against STIs.
What further advice would you give to the girl to help prevent STIs?
That she should ensure that her partner uses a condom, or that she should use female condoms if they are available.
You can help young girls figure out where to keep pills and how to remember to take them at the same time daily by linking pill taking to a routine activity that they do on daily basis. COCs are available in 21-day or 28-day packages (Figure 8.4). Most girls do better using the 28-day pill because it is easier to remember to take a pill every day rather than stopping for 7 days. Carefully discuss with them when they should start taking the pill so that you both are clear about when she begins taking the pills. This will make it easier to determine later whether the pills are being taken correctly.
Do you remember when a woman should begin her daily COCs? (You have learned this in the Family Planning Module.)
A woman can start using COCs any time she wants if it is reasonably certain she is not pregnant. One common way is to start on the first day of menstruation (the monthly period) or the first day after an abortion.
The most important issue is to make sure that young girls understand the necessity of taking pills correctly. Using the knowledge you gained in the Family Planning Module, show the girl the pill packet and explain how to take the pills. Review with her the possible side effects of COCs to make sure that she understands side effects very well and will return to you if she has any problems.
8.2.2 Progestin-only pills (POPs)
POPs are appropriate and safe for young girls. But POPs must be taken daily at approximately the same time every day to be effective in preventing pregnancy, because the progestin levels in the blood peak about two hours after they are taken and then rapidly decline.
If a girl is three hours late taking the pill, she will not be protected and so she should use a back-up form of contraception. POPs may not be the best choice for young girls who cannot remember to take POPs at the same time every day.
POPs are a good choice for girls who cannot tolerate the oestrogen in COCs or have a medical contraindication to the use of COCs.
Stop reading for a moment and think about this from what you learned in the Family Planning Module. What are the medical contraindications to the use of COCs? (You can refer to your Family Planning Module.)
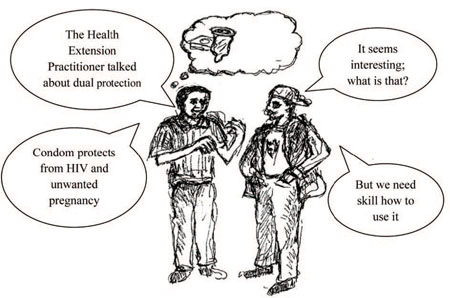
If it is necessary for a girl to switch from a COC to a POP, she should start taking the POP at the end of the active 21 COC tablets. Because POPs do not protect against STIs/HIV, you should encourage condom use in addition to POPs. Remember that this is known as dual protection.
8.2.3 Depo-Provera (DMPA) injectable contraceptive
DMPA (Figure 8.5) is a safe and appropriate method for young girls and is particularly good for those who might have difficulty remembering when to take oral contraceptives. Since it may be difficult for young people to remember to return at regular intervals it may be helpful to use a reminder system that encourages clients to return 12 weeks after the previous injection. This allows for a two-week grace period where the injection can still be given up to 14 weeks without fear of pregnancy. DMPA does not protect against STIs/HIV; therefore you should encourage condom use as well.

8.2.4 Implants
What types of implants do you know that could be used by a young woman. How long does each of them prevent pregnancy?
As you learned in the Family Planning Module, there are two types of implants that are being widely used in Ethiopia. These are: (1) Implanon: one rod, effective for three years, (2) Jadelle: two rods, effective for five years.

Implants (Figure 8.6) are safe and appropriate for young girls and can be safely used by those who are infected with HIV or have AIDS, or are on antiretroviral (ARV) therapy. However you should urge these women to use condoms with implants.
These girls are already infected, so why should they use condoms?
They should use condoms to prevent the spread of infection to their partner and also protect themselves from infection by a new strain of HIV, which the doctors call cross-infection.
You see some of the reasons why young people like implants in Box 8.1 below.
Box 8.1 Why some young girls say they like implants
- Implants do not require the user to do anything once they are inserted.
- Implants prevent pregnancy very effectively.
- They are long-lasting.
- They do not interfere with sex.
Why do you think young people discontinue using implants?
The main reason for the discontinuation of implants is menstrual problems, especially irregular bleeding.
You have learned how you can respond to misconceptions and rumours in the Family Planning Module. Do you remember what misunderstandings on implants exist?
Young people think that implants move to other parts of the body, stop menstrual bleeding, lead to pregnancy outside the uterus (ectopic pregnancy), and make the woman unable to become pregnant even if removed (Figure 8.7).
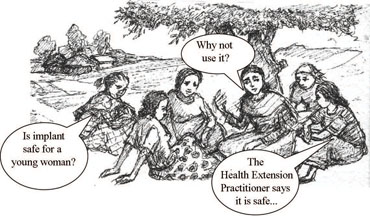
Young girls often have misunderstandings concerning implants. You need to identify what specific misunderstandings they have during your discussion with them on contraceptives and correct them.
Remember it is important to provide information about side-effects, to correct misunderstandings and to give counselling before providing contraception (Figure 8.8).
Why must you give information about side-effects and provide counselling before giving contraception.
The woman may not return to seek your help/advice once she has the implant.
In Box 8.2 below, you see some of the points you can use to correct young people’s misunderstandings about implants.
Box 8.2 Correcting common misunderstandings about implants.
- Implants do not make women infertile.
- Implants stop working once they are removed, and the woman can become pregnant again; after removal of the implant, fertility returns within 4–6 months — or sooner.
- Implants can stop monthly bleeding, but this is not harmful.
- Implants do not move to other parts of the body.
- Implants substantially reduce the risk of ectopic pregnancy.
Counselling is essential because young girls must be prepared for irregular bleeding and must make plans about how they and their partner will react to the irregular bleeding. You should counsel them very thoroughly on the potential side effects of implants, mainly the irregular bleeding.
From your own experience say which type of girls are most likely to choose and use implants?
Girls who select implants are most likely to want three to five years of contraceptive protection, have often experienced failure of other methods, can tolerate a small surgical procedure, and have access to services.
If a young girl chooses to use implants, you should make sure that she will have access to services to remove the implant whenever necessary.
Remember, you should also encourage girls who choose to use implants to use condoms as well because implants do not protect against STIs/HIV.
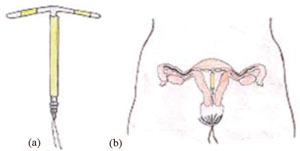
8.2.5 Intra-uterine contraceptive devices (IUCDs)
IUCDs (Figure 8.9) are appropriate for adolescents in stable, mutually monogamous marriages. Women under the age of 20 who have not given birth appear to have greater risk of expulsion and painful menstruation (monthly periods). After you inform them of the characteristics of IUCDs and counsel them, if adolescents who are married would like to use this method, you should refer them to the nearest health centre for further counselling and service provision.
8.2.6 Condoms

Condoms (Figure 8.10) are safe and appropriate for young people. Because they are available without a prescription and provide protection against STIs/HIV, they are a good method. There are male and female condoms, as you have learned in the Family Planning Module.
Young girls frequently are not assertive about the use of condoms when their partner rejects the idea. You should give them ideas about how to negotiate condom use.
Young people often lack the skills to use condoms correctly. You need to develop their skills so that they will use them properly (Figure 8.11).
Activity 8.1
Stop reading for a moment and think of what you have learned from the Family Planning Module. What are the five basic steps of using a male condom? (Figure 8.10 (b)). Write down the five basics steps in your Study Diary.
8.2.7 Other female barrier methods (spermicides, cervical caps, diaphragms)
These female barrier methods are appropriate methods for young people, but they do require a high level of motivation for correct and consistent use. Use is related to intercourse and some young people find this inconvenient or feel it interferes with sexual pleasure.
8.2.8 Lactational amenorrhea method (LAM)

What are the three conditions that must be fulfilled for LAM to be effective?
LAM is appropriate for any young woman who has given birth no more than six months ago, is postpartum, fully or nearly fully breastfeeding (Figure 8.12), and whose periods have not yet returned (she is amenorrheaic). This method may be difficult for young people unless they have a stable lifestyle that is conducive to frequent breastfeeding. The LAM method does not provide protection against STIs/HIV, therefore you should encourage condom use as well.
8.2.9 Female and male sterilisation
While there is no medical reason to deny sterilisation, it is generally not recommended for people at the beginning of their childbearing years. This is because if they decide to have sterilisation, in the future they may be sad about their decision. Once they undergo sterilisation they can have no more children-this is why it is called irreversible contraception. However, there may be mitigating circumstances, such as HIV or the presence of some genetic diseases, which means that a young person may wish to consider sterilisation. Therefore when you encounter a young person who wants to have sterilisation, you should refer them to a higher health facility where further counselling could be provided. Sterilisation does not provide protection against STIs/HIV.
8.2.10 Abstinence

Abstinence is appropriate for young people who have not yet begun sexual activity, as well as those who are already sexually experienced. There may be emotional or social advantages to delaying sexual intercourse until they are older, more mature, or married (Figure 8.13). Abstinence provides protection against STIs and HIV/AIDS.
In the next section you will be able to review what you learned about emergency contraceptives in the Family Planning Module.
8.3 Review of emergency contraceptives (ECs)
In this section we would like you to review a few points about emergency contraceptives to remind yourself of its importance in preventing pregnancy.
What is emergency contraception?
Emergency contraception is a contraceptive method used to prevent pregnancy in the first few days after unprotected intercourse or a contraceptive accident such as leakage or slippage of a condom. These pills used for emergency contraception are also called ‘morning-after’ or ‘post coital’ pills. EC should be given in the first five days after unprotected sex.

Emergency contraceptive pills (ECPs) (Figure 8.14) should be available to young girls who have unprotected sex. The earlier ECPs are taken after unprotected sex, the greater the chances are that they will be effective. ECPs can be provided in advance to young girls so that they could use whenever needed, but they should be counselled that ECPs are for emergency use only. ECPs do not provide protection against STIs/HIV.
8.3.1 Some counselling issues of ECPs

You should consider the following important points when you counsel young people on ECPs. (Figure 8.15)
- Show her the pills and explain how to use them.
- She should swallow the first dose as soon as convenient, but no later than 120 hours after having unprotected sex.
- She should swallow the second dose 12 hours after the first dose. Important: if more than 120 hours have passed since she had unprotected sex, she should not use ECPs.
- If she vomits within two hours of taking a dose, she should take two tablets as soon as possible. If the vomiting occurs after the first dose, she will still need to take a second dose 12 hours later (you can give her extra pills). To reduce nausea she should take the tablets after eating or before bed.
- Instruct her not to take any extra ECPs unless vomiting occurs. More pills will not decrease the risk of pregnancy further.
Important: if more than 120 hours have passed since she had unprotected sex, she should not use ECPs. ECPs do not interrupt or abort an established pregnancy.
- ECPs should not be used as a regular contraceptive method. After use of the ECPs a regular method should be started or resumed if pregnancy is not desired.
- ECPs do not protect from STIs/HIV/AIDS.
- ECPs can be used at any time during the menstrual cycle and more than once during a cycle if necessary.
- Review what to expect after using ECPs. Women will not see any immediate signs showing whether the ECPs have worked. The menstrual period should come on time (or a few days early or late). Tell her that if her period is more than a week later than expected, or if she has any cause for concern, she should return to you.
- Instruct her to return to you when she has her period if she wishes to use a contraceptive method to prevent future pregnancies.
In Box 8.3 we have presented the EC regimen for your review. This will help you provide ECPs for young girls who are in need of ECPs when you have no pre-packed ECPs.
Box 8.3 Emergency contraceptive pills (ECPs) regimen:
There are two types of ECP regimen in use:
- Combined oral contraceptive pills: contain ethinyl estradiol and levonorgestrel or comparable formulations.
- When high-dose pills containing 50 µg (micrograms) of ethinyl estradiol and 0.25 mg of levonorgestrel are available, two pills should be taken as the first dose as soon as convenient, but not later than five days (120 hours) after unprotected intercourse. The second two pills should follow 12 hours later.
- When low-dose pills containing 30 µg ethinyl estradiol and 0.15 mg of levonorgestrel are available, four pills should be taken as the first dose as soon as convenient but not later than five days (120 hours) after unprotected intercourse, to be followed by another four pills 12 hours later.
- Progesterone-only pills:
- When pills containing 0.75 mg of levonorgestrel are available, one pill should be taken as the first dose as soon as convenient, but not later than five days (120 hours) after unprotected intercourse, to be followed by another one pill 12 hours later.
- When pills containing 0.03 mg of levonorgestrel are available, 20 pills should be taken as the first dose as soon as convenient but not later than five days (120 hours) after unprotected intercourse, to be followed by another 20 pills 12 hours later.
Summary of Study Session 8
In Study Session 8, you have learned that:
- Pregnancy before the age of 18 year has several health risks, which include obstructed or prolonged labour, pre-eclampsia (hypertension in pregnancy), unsafe abortion and premature and stillbirth. It also has economic, social and psychological consequences for both girls and boys.
- As pregnancy in adolescence has several bad effects, it is important that adolescents prevent or delay pregnancy through the appropriate use of contraceptive methods.
- Contraceptive methods that are safe and appropriate for adolescents’ use include combined oral contraceptives, progestin-only pills, Depo-Provera (DMPA) injectable contraceptive, implants and condoms.
- IUCDs are appropriate for young people when they are in a stable, mutually monogamous marriage.
- The lactational amenorrhea method is appropriate for a young woman when the following three conditions are fulfilled: under six months postpartum, fully or nearly fully breastfeeding, and amenorrhaeic.
- Abstinence is appropriate for young people who have not yet begun sexual activity, as well as those who are already sexually experienced. As abstinence provides protection against STIs and HIV/AIDS, it is good method for young people.
- Emergency contraceptives should be available for young girls who have unprotected sex but must be used with in the first 120 hours (five days) following unprotected sexual intercourse.
Self-Assessment Questions (SAQs) for Study Session 8
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the questions below. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 8.1 (tests Learning Outcomes 8.1, 8.2 and 8.3)
- a.What are the health consequences that a 16-year-old girl could face if she becomes pregnant?
- b.What should the girl do to prevent or delay early pregnancy?
Answer
- a.Pregnancy before the age of 18 year has several health risks, which include obstructed or prolonged labour, pre-eclampsia (hypertension of pregnancy), unsafe abortion, and premature and stillbirth.
- b.To prevent or delay early pregnancy a 16-year-old girl should abstain from sex. If that is not possible she should use dual protection.
SAQ 8.2 (tests Learning Outcomes 8.1 8.2 and 8.3)
For each of the following contraceptive methods, say whether it is appropriate or not appropriate for a 15-year-old unmarried girl who is sexually active. In each case, explain why it is appropriate or not appropriate.
- a.Combined oral contraceptive pills
- b.Depo provera (DMPA)
- c.IUCD
- d.Sterilisation.
Answer
- a.Combined oral contraceptive pills: appropriate because it has a low failure rate and also offers relief from pain during menstruation.
- b.Depo-provera (DMPA): appropriate because she doesn’t need to remember when to take oral contraceptives; is has a low failure rate.
- c.IUCD: not appropriate because women under the age of 20 who have not given birth appear to have greater risks of expulsion and painful menses due to IUCD.
- d.Sterilisation: not appropriate because she has not yet had a child.
SAQ 8.3 (tests Learning Outcomes 8.1 and 8.3)
For each of the following contraceptive methods, say whether it is appropriate or not appropriate for a 19-year-old married woman who wants to delay pregnancy. Explain why it is appropriate or not appropriate.
- a.Implants
- b.Condom
- c.Lactational amenorrhea method
- d.Abstinence.
Answer
- a.Implants: appropriate because very low failure rate, reversible and long acting.
- b.Condom: appropriate because available without a prescription and provide protection against STIs/HIV.
- c.Lactational amenorrhea method: not appropriate because she doesn’t fulfill the three criteria for LAM.
- d.Abstinence: not appropriate because she is married.
SAQ 8.4 (tests Learning Outcomes 8.1 and 8.3)
What three conditions should be fulfilled if a young woman who has given birth a month ago want to prevent pregnancy by breastfeeding?
Answer
LAM is appropriate for any young woman who is under six months postpartum, fully or nearly fully breastfeeding, and amenorrhaeic.
SAQ 8.5 (tests Learning Outcomes 8.4 and 8.5)
A 17-year-old young woman comes to you saying that she had unprotected sex two days ago and does not want to become pregnant.
- a.What will you give her?
- b.What instructions will you give her?
- c.What important points will you consider when counselling her?
Answer
- a.Emergency contraceptive pills.
- b.Take two pills immediately and the remaining two pills after 12 hours of the first dose.
- c.If vomiting occurs within two hours of the first dose, take the extra pills
- Come back for a regular contraceptive method
- ECPs do not protect from STIs/HIV/AIDS, so she needs to use dual protection.
SAQ 8.6 (tests Learning Outcomes 8.4)
You don’t have any pre-packed ECPs and you have only combined oral contraceptive pills containing 50 µg of ethinyl estradiol and 0.25 mg of levonorgestrel.
- a.How many pills will you give to a girl who is in need of ECPs?
- b.At what interval should she take the pills?
Answer
- a.Two pills should be taken as the first dose as soon as convenient, but not later than five days (120 hours) after unprotected intercourse.
- b.The second two pills should follow 12 hours later.
Notes on Activity 8.1
- Use a new condom for each sex act.
- Before any physical contact, place the condom on the tip of the erect penis with the rolled side out.
- Unroll the condom all the way to the base of the erect penis.
- Immediately after ejaculation, hold the rim of the condom in place and withdraw the penis while it is still erect.
- Dispose of the used condom safely.