Use 'Print preview' to check the number of pages and printer settings.
Print functionality varies between browsers.
Printable page generated Monday, 9 March 2026, 11:31 PM
Communicable Diseases Module: 4. Viral Vaccine-Preventable Diseases
Study Session 4 Viral Vaccine-Preventable Diseases
Introduction
In Study Session 3 we gave an overview of vaccine-preventable diseases, and then focused on two of the main diseases in this category that are caused by bacteria. In this study session, you will learn about the major vaccine-preventable diseases that are caused by viruses, how they are transmitted, and how they can be prevented and controlled. Knowing the signs and symptoms of these viral diseases will help you to identify them in your community, so that you can refer infected people quickly for treatment at a nearby health centre. Greater understanding of viral vaccine-preventable diseases will also enable you to explain to parents why they should have their children vaccinated to prevent them from susceptibility to these viruses. How to give vaccines to children is described in the Immunization Module.
Learning Outcomes for Study Session 4
When you have studied this session, you should be able to:
4.1 Define and use correctly all of the key words printed in bold. (SAQs 4.1 and 4.3)
4.2 Describe what causes the common viral vaccine-preventable diseases, how the infectious agents are transmitted, and the characteristic signs and symptoms of an affected person. (SAQs 4.2 and 4.3)
4.3 Describe the treatment in the community of children who have measles. (SAQ 4.2)
4.4 Describe how measles, polio and hepatitis B can be controlled and prevented in rural communities. (SAQ 4.3)
4.1 Overview of viral vaccine-preventable diseases
As you know from Study Session 1 of this Module, viruses are microscopic infectious agents that do not have the structure of a cell; they are more like tiny boxes or particles. They are much smaller than bacteria and can only be seen with the most powerful microscopes. Some of the diseases caused by viruses can be prevented by vaccination, as you will learn in this study session.
Do you know of any human communicable diseases caused by a virus?
HIV disease and AIDS are caused by the human immunodeficiency virus (HIV). You may also have thought of measles, polio or hepatitis.
HIV cannot be prevented by vaccination at the present time, but the other three viral diseases mentioned above are part of the Expanded Programme of Immunization (EPI) in Ethiopia and many other countries around the world (see Table 4.1). The composition of the vaccines, which contain dead or weakened viruses or fragments of their structure, and the routes of administration, are described in detail in the Immunization Module. In the following sections, we will look at each of these diseases in turn.
| Disease | Cause | Mode of transmission | Symptoms | Prevention methods |
|---|---|---|---|---|
| Measles | measles virus | Respiratory by coughing or sneezing | Cough, rash and fever | measles vaccination |
| Poliomyelitis | polio virus | Ingesting (faeco-orally) | A few children have paralysis of the legs or hands; many will not show symptoms | oral polio vaccination (OPV) |
| Hepatitis | hepatitis B virus | Direct contact with body fluids or blood, or sexually transmitted | Fever, yellow colouring of the white part of the eye; many children will not show symptoms | hepatitis B vaccination |
4.2 Measles
In this section, you will learn about what measles is, how it is transmitted, what its signs and symptoms are, and how it can be treated and prevented. Having this information will help you to identify a child with measles and give necessary treatment. After reading this section, you should also be able to identify an epidemic of measles in the community if it occurs, so you will be able to report it to the District Health Office.
4.2.1 Definition, cause and occurrence of measles
Note that (unlike bacteria, which have two-part species names) the names of most viruses are simply the disease it causes followed by the word ‘virus’, as in ‘measles virus’.
Measles is a highly transmissible infectious disease caused by the measles virus. Globally, measles kills more children than any other vaccine-preventable disease. In 2008, there were around 165,000 deaths from measles worldwide – most of them in young children and almost all of them in low-income countries. Because the virus is so easily transmitted, you should be aware that it usually causes an epidemic and may cause many deaths, especially among malnourished children. In Ethiopia, measles occasionally causes epidemics. Almost 5,000 children suffered from measles in 2009 and 2,726 cases had already been confirmed in 2010 by early July of that year. However, it is estimated that deaths from measles can be reduced by more than 60% through effective vaccination programmes.
4.2.2 Mode of transmission of measles

Measles is spread through contact with the nose and throat secretions of infected people, and in airborne droplets released when an infected person sneezes or coughs. A person with measles can infect others for several days before and after he or she develops symptoms. The disease spreads easily in areas where infants and children gather, for example in health centres, homes and schools (Figure 4.1).
4.2.3 Clinical manifestations of measles
The first sign of infection with measles is a high fever, which begins approximately 10–12 days after exposure to the virus and lasts for several days. During this period, the child may develop a runny nose, a cough, red and watery eyes (Figure 4.2), and small white spots inside his or her cheeks.

Conjunctivitis is pronounced 'con-junk-tiv-eye-tiss'.
After several days, a slightly raised rash (appearance of small pigmentations or red spots on the skin, or ‘shifta’ in Amharic), develops, usually on the face and upper neck. Over a period of about three days, the rash spreads to the body (Figure 4.3) and then to the hands and feet. It lasts for five or six days and then gradually fades. The incubation period from exposure to the onset of the rash averages 14 days.

To identify cases of measles, you need to confirm the presence of fever and rash, with cough or running nose, or conjunctivitis (red eyes).
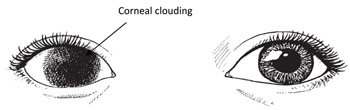
Measles may be severe, causing several complications that can lead to permanent disability or death, including pneumonia (infection of the lower respiratory tract), encephalitis (infection in the brain), otitis media (infection of the middle ear), corneal clouding and blindness (Figure 4.4), and diarrhoea with dehydration. You will learn about pneumonia and acute otitis media in more detail in Study Session 35.
The structure of the eye and the main causes of blindness are covered in the Module on Non-Communicable Diseases, Emergency Care and Mental Health.
Severe measles, manifested by complications such as pneumonia, and clouding of the eyes or blindness, is particularly likely in poorly nourished children, especially those who do not receive sufficient vitamin A in their diet. Vitamin A, which is found in yellow vegetables like carrots and yellow fruits like mangoes, is essential for good eyesight and it also strengthens the immune system of children. If measles develops in a child with a shortage of vitamin A, this makes the disease more severe and damage to eyesight is more likely. Measles and vitamin A deficiency together are a major cause of blindness among children in Africa and in other areas of the world where measles is common. Children who live in crowded conditions and whose immune systems have been weakened by HIV/AIDS, or other diseases, are also more likely to develop severe measles.
Give a reason why malnourished children are more likely to develop severe measles.
Children with malnutrition, particularly those who lack vitamin A, have weak immunity and cannot fight the measles virus, which causes severe clinical symptoms and may even kill them.
4.2.4 Treatment, prevention and control of measles
![]() Cases of severe measles with pneumonia or clouding of the cornea should be referred immediately to the nearest health facility.
Cases of severe measles with pneumonia or clouding of the cornea should be referred immediately to the nearest health facility.
It is very important to encourage children with measles to eat and drink. Advise the parents to help their child as much as possible with nutrition and intake of fluids; treat any dehydration with oral rehydration salts (ORS) as necessary. Antibiotics should only be prescribed for ear infections and pneumonia caused by bacteria, which are able to develop in the person weakened by measles. Remember that antibiotics only attack bacteria – they have no activity against any viruses, including the measles virus.
Vitamin A supplementation
As lack of vitamin A is such a problem associated with measles, all children in developing countries who are diagnosed with measles should receive two doses of vitamin A supplements given 24 hours apart, at a dosage appropriate to their age (see Table 4.2). For instance, a 7 month-old infant with measles should receive one dose of vitamin A, which contains 100,000 International Units (IU) on the day of diagnosis (day 1) and also on the next day (day 2). Giving Vitamin A can help prevent eye damage and blindness and reduce the number of deaths from measles by 50%, so this is a very important and effective part of the treatment.
IU stands for International Unit; this is the internationally agreed measurement of vitamin dosages
| Age | Immediately on diagnosis | Next day | Follow-up |
|---|---|---|---|
| Infants less than 6 months old | 50,000 IU | 50,000 IU | Third dose 2–4 weeks later if there are signs of eye problems |
| Infants aged 6–11 months | 100,000 IU | 100,000 IU | |
| Children aged 12 months and over | 200,000 IU | 200,000 IU |
Measles vaccination
How to administer the measles vaccine to children is described in the Immunization Module.
Measles is prevented by vaccination with measles vaccine. By the year 2008, successful vaccination campaigns all over the world had succeeded in reducing measles deaths by around 75% — a huge drop from the 750,000 deaths in the year 2000. The World Health Organization (WHO) estimated that in 2008 around 83% of the world’s children were receiving one dose of measles vaccine by their first birthday.
All infants at nine months of age or shortly thereafter should be vaccinated through routine immunization services. This is the foundation of the sustainable measles death-reduction strategy. It is also possible to reduce infections with measles by giving vaccination to vulnerable children. For example, to reduce the risk of measles infection in hospitals, all children between the ages of six and nine months, who have not received measles vaccine and who are admitted to a hospital, should be vaccinated against measles. If the children’s parents do not remember or know whether they have received measles vaccine, the child should still be vaccinated. If a hospitalised child has received measles vaccine before nine months of age, a second dose should be administered at nine months, or as soon as possible after nine months.
All children should be provided with a second opportunity for measles vaccination. This is to make sure that children who did not receive a previous dose of measles vaccine, or children who were vaccinated earlier but did not develop immunity, have another chance to develop immunity. The second opportunity may be delivered either through routine immunization services or through periodic mass campaigns of vaccination.
Measles surveillance
Measles surveillance (looking for cases of measles in the community) should be strengthened at community level, so that there is early warning of any possible epidemics. Try to persuade parents that a child with measles should be kept isolated from other children who have not previously had measles or been vaccinated, to avoid the disease from spreading. As a health worker, you should report any cases of measles in your community to the District Health Office. As well as this, of course, you have the important task of vaccinating all children who are around nine months old against measles.
Next, we would like you to read Case Study 4.1 and then answer the questions that follow it.
Case Study 4.1 Alemu’s parents want to cure his rash by prayer
During a house-to-house visit in a remote village, you see a one year-old boy called Alemu, who has a high fever, a cough and small rashes (the spots look like teff) on his forehead and neck. Alemu’s parents call this illness ‘ankelis’ or ‘wotetie’ in the local language. The treatment they believe will cure their son is to prepare a coffee ceremony to the gods who they believe to have spiritual power. They informed you that their two older children were cured by the same treatment and they will continue acting the same way for Alemu.
What should you advise Alemu’s parents? What actions should you take to help the child? And what else should you do?
Advise the parents that the child may have a disease called measles, which is caused by a virus. Measles is prevented by vaccination, and children who recover from measles naturally will never get it again (they develop lifelong immunity). If the disease is severe, children may die. Inform the parents that for a very sick child like Alemu, complications such as pneumonia and death can be prevented by giving vitamin A and fluids such as oral rehydration salts. Give vitamin A (200,000 IU) on the first and second day to Alemu. After convincing the parents, refer the child to the health centre and report the case to the District Health Office. Search for other similar cases in the village.
4.3 Poliomyelitis (polio)
In this section, we will describe what polio is and how it is transmitted, its clinical symptoms, how it is treated and how it can be prevented and controlled. This will help you to identify cases of polio and refer them for further diagnosis and treatment. It will also help you to give health education in your community about how to prevent polio in children through the administration of oral polio vaccine in drops into the mouth.
4.3.1 Definition, cause and occurrence of polio
Poliomyelitis (usually called polio) is a viral disease that causes paralysis (weakness or inability to use the muscles) of the legs, arms or hands. Polio is caused by three types of viruses, namely, poliovirus types 1, 2 or 3; (note that ‘poliovirus’ is all one word). Many countries agreed in 1988 to try to eradicate polio completely from the world. The Ethiopian government has a plan to eradicate the disease in the near future. As a result of a continuing vaccination programme, polio is fortunately becoming a rare disease in Ethiopia. However, there are sometimes cases among people who come to Ethiopia from neighbouring countries such as Sudan.
4.3.2 Mode of transmission and clinical manifestation of polio
Polioviruses are transmitted when people drink water or eat food contaminated by faeces (or stools) which carry the virus (faeco-oral transmission). However, most children infected by polioviruses never feel ill. Less than 5% of those infected may have general flu-like symptoms such as fever, loose stools, sore throat, headache, or stomach ache. Most children who get a poliovirus infection without symptoms develop immunity and have lifelong protection against polio. A few children may develop a kind of paralysis called acute flaccid paralysis (AFP), which is characterised by acute (rapidly developing, severe) loss of movement or weakness of the legs, arms or hands.
Paralytic polio begins with mild symptoms and fever, followed by severe muscle pain and paralysis, which usually develops during the first week of illness. Patients may lose the use of one or both arms or legs. Some patients may not be able to breathe because of the paralysis of respiratory muscles in the chest, which can lead to death. Some patients who develop paralysis due to polio recover the ability to move the affected limbs to some degree over time, but the degree of recovery varies greatly from person to person. A diagnosis of polio is confirmed by laboratory testing of stool samples.
4.3.3 Treatment and prevention of polio
While the initial symptoms of acute polio such as muscle pain and fever can be relieved, there is no treatment that can cure the weakness and paralysis if AFP develops. Regular physical exercise can help paralysed children to resume some activity. Prevention of polio by vaccination is the best method to eradicate the disease. Three doses of oral polio vaccine (OPV) are given during routine vaccinations for other communicable diseases, and/or during campaigns for polio eradication. A detailed description of the vaccination procedure is given in the Immunization Module.
An initial dose of OPV can also be given at birth or before 2 weeks of age.
Polio surveillance and reporting
You should immediately report a case of AFP to the District Health Office and take stool samples from the patient. The stool sample should be sent to Addis Ababa to identify the virus. Stool specimens must be collected within 14 days of paralysis onset in order to have the greatest chance of isolating the virus. Try to collect the first specimen at the time of the case investigation. If the patient is not able to produce a stool, leave a cup, cold box and frozen ice packs with the family so that they can collect it from the patient later.
To collect faeces from the child, ask him or her to defaecate onto clean paper. Use a spatula or very clean spoon to put the stool specimen in a clean container and label it and write the date. After collection, the specimens must be placed immediately in a refrigerator for shipment, or in a cold box between frozen ice packs at 4–8°C. The specimens must reach the laboratory in Addis Ababa within 72 hours of collection.
Gemechis is a two-year-old boy who has had weakness in his legs for the last two days. His mother has told you that he has mild fever and diarrhoea. What should you do?
The boy may have AFP due to poliovirus infection. You should collect a stool sample from Gemechis and immediately report to the District Health Office and have the sample sent to Addis Ababa for laboratory analysis. For further evaluation and treatment, refer the child to the nearest health centre.
As a Health Extension Practitioner, if you identify a case of AFP you must report it immediately. You will also routinely need to give the oral polio vaccine (OPV) to all eligible children in your community.
4.4 Hepatitis B
In this section, we describe what hepatitis B is and how it is transmitted, its clinical symptoms, and how it can be treated and prevented. This will help you to identify cases of hepatitis and refer them for further investigation and treatment, and also to educate your community about what causes hepatitis B and how it can be prevented by vaccination and safer sexual practices.
4.4.1 Definition, cause and occurrence of hepatitis B
Hepatitis is a term referring to a serious inflammation of the liver. Several viruses can cause hepatitis, but the hepatitis B virus (or HBV) is the most important one. Hepatitis B disease is a major global health problem and the most serious type of viral hepatitis. The WHO estimates that an estimated two billion people have been infected with HBV worldwide, and more than 350 million have chronic (long-term) liver infections. About 600,000 people die every year as a result either of acute liver infection, or of chronic liver damage or liver cancer, which develops slowly over decades and eventually leads to their death.
4.4.2 Mode of transmission and clinical manifestation of HBV
HBV is carried in the blood and other body fluids of people who are infected. It is usually spread by contact with infected blood or body fluids in the following ways:
- Injury or injection: with contaminated sharp unsterile objects or instruments.
- From a pregnant mother to her baby: During birth, the virus which exists in the blood or body fluid of the mother may be transmitted to the baby.
- Unprotected sexual intercourse: During sexual intercourse without a condom, the virus which exists in the blood of the infected person may be transmitted to the other partner through scratches or wounds, or through small breaks in the delicate membranes covering the sexual organs.
The incubation period of hepatitis B averages six weeks, but may be as long as six months. Young children who are infected (usually at birth) often show no symptoms. Also, a larger proportion of children become chronic carriers of HBV, compared with infected adults.
Do you remember what a ‘chronic carrier’ means?
It is a person who carries the infection for a long period of time and can transmit the infectious agent to others, but without showing any symptoms of the disease themselves.
People who show symptoms of hepatitis B disease may feel weak and experience stomach upsets and other flu-like symptoms, which may last several weeks or months. They may also have very dark urine or very pale stools. Jaundice, which presents with yellowing of the skin or a yellow colour in the whites of the eyes (Figure 4.5), is common. Jaundice results when the liver is unable to deal with a yellow substance called bilirubin, which is formed when old red blood cells are broken up and their constituents are recycled to make new red blood cells. If the liver is damaged, it can’t deal with the bilirubin, which builds up in the body causing the yellow discoloration.
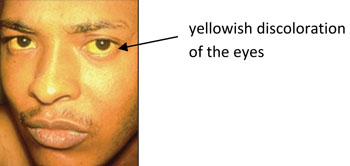
A laboratory blood test is required for confirmation of hepatitis B infection. Most HBV infections in adults are followed by complete recovery and 90% of adults will be completely rid of the virus within six months. Recovery also means that they are naturally protected from further infection with HBV for the rest of their lives. However, 30–90% of infants and children who become infected with HBV become chronic carriers of the virus, and they have a much increased risk of developing chronic, life-threatening liver damage or liver cancer much later in life.
4.4.3 Treatment, prevention and control of hepatitis B
You should be aware that there is no curative treatment for acute hepatitis B disease. Advise patients or the parents of affected children to try to keep eating and drinking; replacement of fluids lost through vomiting or diarrhoea is essential, and giving ORS is recommended if dehydration is a concern. In chronic hepatitis B infection, the disease can sometimes be halted with medication, but the drugs cost thousands of dollars and are rarely available in developing countries.
The pentavalent vaccine and its administration is described in the Immunization Module.
Prevention of hepatitis B disease is by vaccination, which is 95% effective. All infants should get three or four doses of hepatitis B vaccine during the first year of life, as part of routine vaccination schedules. In Ethiopia, it is usually given in the pentavalent vaccine, which protects against HBV and four bacterial diseases. Your role is to educate your community about how hepatitis B is transmitted and how transmission can be avoided, and you will need to give the pentavalent vaccine to infants.
Do you know another viral disease which has the same modes of transmission as hepatitis B? What health education messages can you give to people to protect themselves from both diseases?
HIV has the same modes of transmission as HBV. The advice on protection from acquiring both these viruses is to avoid contact with another person’s blood or body fluids, particularly during sexual intercourse.
Ways to prevent transmission of HIV are described in detail in Study Session 26 of this Module; they also apply to prevention of HBV transmission.
In the rest of Part 1 of this Communicable Diseases Module (Study Sessions 5–12), you will be learning about a disease that cannot (at the present time) be prevented by vaccination, which is not caused by either bacteria or viruses. It is the vector-borne disease malaria, caused by a protozoan and transmitted by mosquitoes.
Summary of Study Session 4
In Study Session 4, you have learned that:
- Measles, polio and hepatitis B are viral vaccine-preventable diseases; most infants and children are protected from these infections in Ethiopia and most other countries by routine vaccinations.
- Measles virus is easily transmitted from person to person by the respiratory route. Typical symptoms include fever, cough, running nose, red eyes, diarrhoea and a widespread rash. Severe measles may lead to complications such as ear infections, loss of eyesight and pneumonia.
- Vitamin A should be given to children with measles to prevent damage to the eyes, which may lead to blindness.
- Poliomyelitis (caused by poliovirus) is transmitted from person to person through the faeco-oral route. Most children with polio infection do not show symptoms, but a few may develop acute flaccid paralysis (AFP).
- Hepatitis B virus (HBV) has several routes of transmission, such as contact with infected blood or other body fluids, through wounds, from mother to child at birth, or during unprotected sexual intercourse.
- People with hepatitis B present with fever, weakness and jaundice. Children infected with HBV may become chronic carriers; long-term complications such as permanent liver damage or liver cancer can develop in later life.
- Cases of measles, AFP and hepatitis should be actively searched in the community and reported to the District Health Office. Diagnosis can only be confirmed by laboratory isolation of the viruses.
- Patients with severe complications of measles, AFP or signs of hepatitis, should be referred to the nearest health centre.
- There is no curative treatment for measles, polio or hepatitis B disease. Supportive treatment for reduction of symptoms of measles and hepatitis includes maintaining intake of nutrients and fluids. Exercise therapy may help to improve mobility in people with AFP.
Self-Assessment Questions (SAQs) for Study Session 4
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 4.1 (tests Learning Outcomes 4.1, 4.2 and 4.4)
Which of the following statements is false? In each case, explain what is incorrect.
A Pneumonia and clouding of the cornea are two of the common complications of severe measles.
B Measles is very rarely fatal.
C The transmission of poliovirus cannot be prevented at the present time.
D Acute flaccid paralysis (AFP) is a rare complication of polio; most children infected with poliovirus show no symptoms.
E Almost all adults infected with hepatitis B virus (HBV) become virus carriers for the rest of their lives.
F Jaundice is a common complication of hepatitis B disease.
Answer
A is true. Pneumonia and clouding of the cornea are two of the common complications of severe measles.
B is false. Measles can be fatal, particularly in malnourished children. Around 165,000 children died of measles worldwide in 2008.
C is false. The transmission of poliovirus is easily prevented by routine vaccination of all children. The aim is to eradicate polio totally from the world by this measure.
D is true. Acute flaccid paralysis (AFP) is a rare complication of polio; most children infected with poliovirus show no symptoms.
E is false. 90% of adults infected with hepatitis B virus (HBV) will get rid of the virus from their bodies within six months.
F is true. Jaundice is a common complication of hepatitis B disease.
SAQ 4.2 (tests Learning Outcomes 4.2 and 4.3)
You see a child in your village who has a rash all over his body, which developed three days ago; before that he was ill with fever and diarrhoea, his nose was running and his eyes were red. Now he has an ear infection, with pus coming out of his ear. What is the most likely cause of his illness? What do you do in response?
Answer
The child is showing the characteristic signs of measles, and in his case the ear infection shows the illness is severe. For severe measles cases, give the child the first dose of vitamin A according to his age, and refer him immediately to the nearest health centre. He may need antibiotics to treat the ear infection and prevent other complications.
SAQ 4.3 (tests Learning Outcome 4.2)
In Table 4.2 below, write the mode of transmission and the method of prevention against each of the viral diseases in the first column.
| Disease | Mode of transmission | Prevention |
|---|---|---|
| Measles | ||
| Polio | ||
| Hepatitis B |
Answer
The completed version of Table 4.2 is shown below.
| Disease | Mode of transmission | Prevention |
|---|---|---|
| Measles | Respiratory Route | Measles vaccination and vitamin A drops |
| Polio | Faeco-oral route | Oral polio vaccination |
| Hepatitis B | Unprotected sex or other contact with infected blood or body fluids | Hepatitis B vaccination |