2 What is AMR?
As noted in other modules, this course focuses on bacteria and will generally use AMR to mean bacterial resistance to antibiotics, but strictly speaking, AMR encompasses all the different micro-organisms.
Antimicrobials are used to treat infections in humans, animals (terrestrial and aquatic, companion and food-producing), and plants (crops, fruit trees, ornamental, etc). As antimicrobial resistance is a growing global issue across all sectors and since antimicrobials used in one sector can contribute to the emergence and spread of AMR in other sector(s), a ‘One Health approach’ is needed to fight AMR. (See more on One Health in the module Introducing a One Health approach to AMR.)
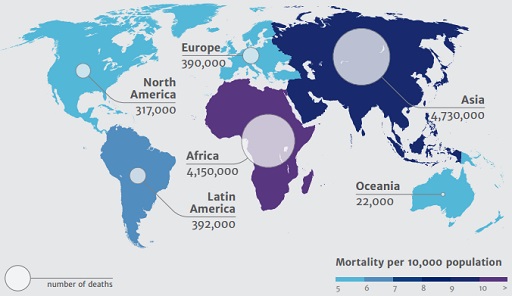
It is clear that antimicrobial resistance is an unavoidable evolutionary consequence of the selective pressure resulting from the use of antimicrobials. However, strategic decision-making and coordinated action at local, national and global levels to promote the prudent use of antimicrobials is key to mitigate the spread of resistance and the resulting morbidity and mortality. Figure 1 below, taken from the Review on Antimicrobial Resistance (also referred to as the O’Neill Report) highlights the projected mortality in humans in 2050 as a consequence of AMR.
1 How do we define surveillance?