2.1.1 Use of antimicrobials in animals selects for resistance
The ways in which the use of antimicrobials in animals can influence the emergence of AMR are illustrated in Figure 5.
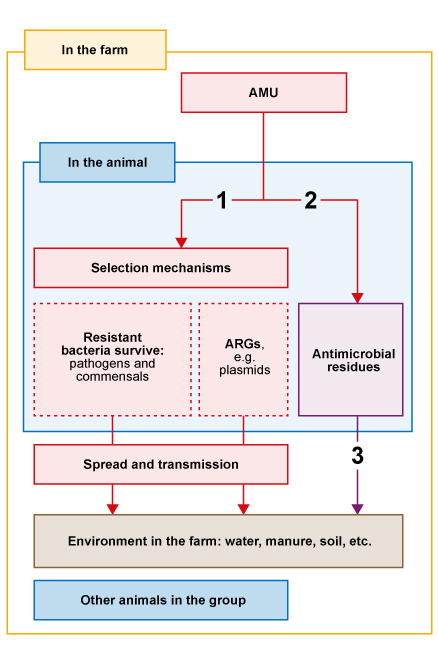
The three pathways in Figure 5 act as follows:
- AMU speeds up the selection of resistant bacteria and
antimicrobial resistance genes (ARGs) . In the animal, bacteria with genes that confer resistance to the antimicrobial administered will survive when they are exposed to that antimicrobial. Resistant bacteria multiply in the animals, especially in the gut. Resistant bacteria and ARGs are shed into the environment where they can spread to other animals by routes such as direct contact and faeco-oral transmission. Transmission is more likely in conditions of high stocking density and poor hygiene. - Antimicrobials given to animals can persist as breakdown products or
residues in the animal for varying lengths of time, depending on the specific drug, dose and route of administration. Thewithdrawal period is the minimum period of time allowed between the last administration of a specific drug to an animal, and the collection of edible tissue or products from the animal. It ensures that the residues in food comply with the maximum residue limit for that specific drug (Codex Alimentarius, 1993). - In addition, antimicrobials may be excreted in the urine or faeces to the environment. Excretion can be due to incomplete absorption of oral drugs, or excretion of drugs (or their
active metabolites ) given by non-oral routes. These excreted drugs or their metabolites are known as residues. An active metabolite is a version of the drug that has been chemically changed by the body but still has some antimicrobial properties.
2.1 Introduction to AMR in animal health