3 The pre-analytical stage
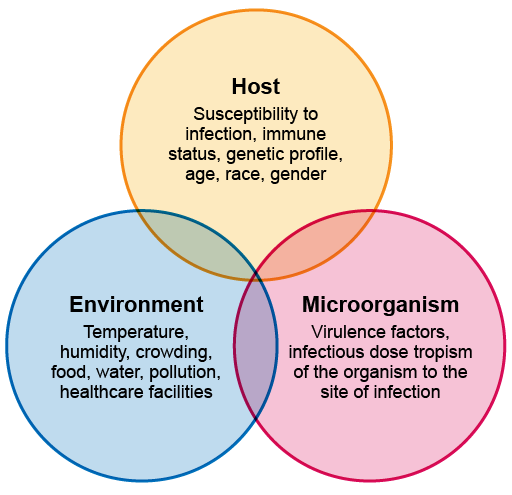
The clinical presentation of an infectious disease reflects the interaction between the host, the microorganism and the environment. When they are assessing a patient, the clinician – who could be a doctor, clinical officer, nurse, physician associate, community healthcare worker, etc. – needs to consider:
- the patient’s history and reported symptoms
- any physical findings
- any risk factors that might pre-dispose them to particular infections, such as whether they are immunosuppressed, what diseases are prevalent locally or any occupational exposures.
A clinician must also consider any local outbreaks of diseases such as cholera, or disease outbreaks in healthcare facilities related to antimicrobial-resistant organisms. For AMR, a history of recent healthcare exposure and whether or not the patient has recently taken antimicrobials is also important, because these are risk factors for resistant infections.
Signs and symptoms also vary according to the site and severity of infection; they may be localised or systemic, with fever, chills and hypotension. For example, patients with an uncomplicated UTI may have localised symptoms such as pain on passing urine; but if the infection is more severe and involves their kidneys, they may have back or loin pain, fever and chills, weakness and tenderness, and are likely to be unwell. Patients with bloodstream infections are likely to be very unwell, with systemic fever and low blood pressure.
The origin of the infection also needs to be considered.
Figure 3 gives an overview of these interactions.
Although this modules focuses on bacterial infections, you should remember that patients presenting with fever may have other types of infection, and the history and examination should consider all the possible infection types. Again, the patient’s exposure history and information about local
2 The diagnostic workflow in the clinical microbiology laboratory