1.1 Targeting priorities
Improving the use of antimicrobials through
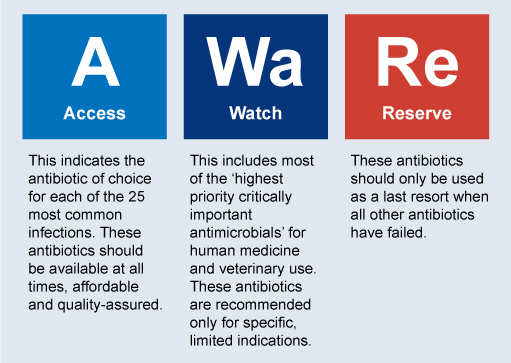
For that reason, WHO in 2017 introduced the Access, Watch, Reserve (
(The concepts of AMU and AMC data, and how each differ, is explained in the Introducing AMR surveillance systems module.)
Quantifying AMU in each of the AWaRe categories allows some inference about the overall quality as well as quantity of AMU. For example, overuse of antimicrobials in the Watch group can become immediately apparent: activities to reduce the use of these antimicrobials and promote the use of drugs in the Access category can be identified as targets for AMS interventions. These trends can be assessed over time to evaluate the impact of the stewardship interventions.
Case Study 1 is a good illustration of how AMS programmes are often initiated in facilities or even countries due to an outbreak of multidrug-resistant bacteria.
Case Study 1: Facility AMS in Barbados (WHO, 2019b)
An outbreak of carbapenemase-resistant Klebsiella pneumoniae (KPC) in a 600-bed healthcare facility in Barbados led to an AMS programme being established.
At the time of the outbreak, the facility’s infection prevention and control (IPC) programme consisted of a single nurse; this was later expanded to include an infectious disease physician and a pharmacist. The IPC team used data to demonstrate to the hospital management that an AMS programme was critically needed and that it would involve minimal cost.
Leadership commitment led to establishing an AMS team consisting of an infectious disease physician, a pharmacist and a microbiologist, as well as IPC-trained personnel who were all already employed in the facility.
The AMS set a target for decreasing the overall cost of antibiotics and hospital length of stay over the next six to twelve months. The targets were achieved faster than anticipated, and interest grew from other wards to be included in the AMS programme. A 60% decline in the use of carbapenems and vancomycin was documented.
Case Study 1 demonstrates the importance of communicating AMR and AMU data to improve AMS. The IPC team used data to communicate the need for an AMS programme to hospital management. The AMS programme achieved a 60% decline in use of several Watch antibiotics (carbapenems and vancomycin).
Certain stakeholder groups will play an important role in influencing the use of antimicrobials:
- those who prescribe (such as healthcare workers or veterinarians)
- those who dispense (such as pharmacists, retailers and veterinarians)
- those who consume (such as patients, or farmers treating plant and animal infections).
Each of these groups requires bespoke messaging and targeted strategies. Priority-setting helps to pinpoint where efforts should be focused for the greatest impact and return on investment.
Activity 2: Communication in AMS programmes
1 Making an impact with AMR data