18.1 Malaria in pregnancy
Malaria is an infection of the red blood cells caused by a parasite called plasmodium that is carried by certain kinds of mosquitoes. A mosquito sucks up the malaria parasites in the blood of an infected person when it takes a blood ‘meal’, and then passes the parasites on when it bites someone else (Figure 18.1). The parasites develop to maturity in the person’s red blood cells and millions of parasites collect in the placenta of a pregnant woman.
Malaria can be more severe in women who are sick with other illnesses. Malaria is more dangerous to pregnant women than to most other people. A pregnant woman with malaria is more likely to develop anaemia (as you will see later in this study session), have a miscarriage (spontaneous abortion of the fetus before 24 weeks of pregnancy), an early birth, a small baby, a stillbirth (baby born dead after the 24th week of pregnancy) or to die herself (maternal mortality).
18.1.1 Symptoms of malaria
The symptoms of a disease are the indications that an affected person is aware of and is able to tell you about; they may tell you spontaneously, but you may have to ask the right questions. The symptoms of malaria are:
- Chills (feeling unusually cold, shivering) and rigors (intense periods of shivering lasting several minutes and up to 1 hour); this is often the first symptom of an attack
- Headache and weakness often accompany the chills
- Fever (raised temperature); the fever often follows the chills, and the temperature may go so high that the person suffers delirium (not being in her right mind, seeing or hearing things that are not real)
- Sweating as the temperature falls
- Diarrhoea/vomiting may also be experienced in some cases
- Muscle/joint pain is another common symptom.
The periods of fever typically alternate with periods of chills and rigors in attacks that can occur every day, or every 2-3 days. All of these symptoms could be due to something else, but you should suspect malaria if they happen in a person who has been exposed to mosquitoes in an area where malaria is known to occur.

The signs of a disease are the indications that only a trained health professional would notice, or be able to detect by conducting a test. For example, if you suspect malaria, you should take the person’s temperature with a thermometer if you have one (you learned how to do this in Study Session 9), or by comparing your own temperature with the woman’s (Figure 18.2). In cases of malaria, the fever can go as high as 39-40°C or even higher.
What is the normal body temperature and what would be a sign of fever?
Normal body temperature is 37oC; a sign of fever would be a temperature of 38oC or above.
18.1.2 Diagnosis of malaria
There are two main ways to diagnose malaria using blood tests. The simplest way is to run a malaria rapid diagnostic test (RDT), which detects proteins produced by the parasite in the patient’s blood. The test kits can be in the form of a dipstick, a plastic cassette or a card, which changes colour when exposed to a drop of blood from an infected person – usually taken by pricking a finger with a sterile lance. However, the test kits must be stored carefully and protected from humidity and high temperatures. Training for health workers is required before the signs of malaria in the test results can be interpreted accurately.
The other way to diagnose malaria, which requires specialist training and equipment, is from microscopic examination of a smear of blood on a glass slide, which has been stained to reveal the parasites. Facilities for microscopic blood testing are usually not available at Health Post level. If you have been trained to use the malaria RDT and have access to properly stored test kits, you should diagnose malaria on the basis of the test results. If you are unable to use the malaria RDT, base your diagnosis on the symptoms (e.g. headache, fever, chills, muscle/joint pain), and high temperature measured with a thermometer.
18.1.3 Treatment of malaria in pregnancy
It is important for pregnant women to avoid malaria — or to be treated quickly if they get sick. Malaria medicines can have side-effects, but these medicines are much safer than actually getting sick with malaria. If a woman has symptoms of malaria, she should be treated right away. The medicine used in Ethiopia in the Health Extension Programme is called Artemether Lumifantrine (marketed as Coartem tablets). It works by interfering with the development of the parasites in the person’s red blood cells.
Coartem can be used to treat malaria during the second and third trimesters of pregnancy. The second trimester is 13-27 weeks since the woman’s last normal menstrual period (LNMP), and the third trimester is from 28 weeks until the birth at around 40 weeks. If the diagnostic test is positive for malaria, or you strongly suspect malaria based on the clinical signs and symptoms, and the woman is in either the second or third trimester, treat her as indicated in Box 18.1.
Box 18.1 Coartem treatment in the second or third trimester of pregnancy
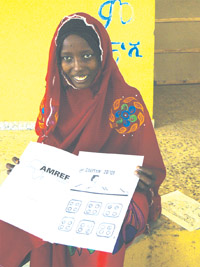
- Four Coartem tablets twice a day (12 hours apart) for 3 days (a total of 24 tablets). Tell her to take the tablets with food, milk, oatmeal or soup. She can crush them and mix them with a spoonful of food if this makes it easier for her to swallow the medicine. Figure 18.3 shows a way of explaining to women how many tablets to take.
- You can also give her paracetamol tablets (500-1000 mg) every 4-6 hours to bring down her temperature when she has a fever.
- Cold sponging her body with a cloth dipped in cool water will also help when she has a fever.
- Advise the woman to drink plenty of fluids to make sure she does not become dehydrated. She should drink at least 1 large cup of fluid every hour.
![]() Pregnant women with suspected malaria in the first trimester, who are not too sick to travel, should be referred to the nearest health centre for specialist treatment.
Pregnant women with suspected malaria in the first trimester, who are not too sick to travel, should be referred to the nearest health centre for specialist treatment.
If the woman is in the first trimester (i.e. up to 12 weeks since her LNMP), but she is too sick to travel to the health centre, give her the treatment in Box 18.2. The risk from malaria to her life and the life of her fetus is greater than the risk from taking the medicine during early pregnancy. Send her to the health centre as soon as she is well enough to travel. Note that the drug Artesunate is given by slipping a specially shaped capsule — called a suppository — into the woman’s rectum by pushing it gently through her anus.
Box 18.2 Artemether injection and rectal Artesunate
Pre-referral intramuscular (IM) injection of Artemether is given in cases of severe suspected malaria. The dosage is 3.2 mg of Artemether for every kilogram (kg) of the woman’s body weight, in a single injection into the muscles of her upper arm.
Pre-referral rectal Artesunate given in suppositories with the following doses.
| Woman’s weight | Dose | Number of suppositories |
|---|---|---|
| 30-39 kg | 50 mg | 1 |
| over 40 kg | 400 mg | 4 |
Note that pregnant women are likely to weigh more than 40 kg after the first trimester.
The total number of malaria deaths and cases has been falling in Ethiopia in recent years, due to the major effort to prevent the disease and to treat it rapidly when it occurs. The Health Extension Programme is vitally important in reducing malaria even further, including early diagnosis and treatment of pregnant women coming to you for antenatal care.
18.1.4 Prevention of malaria
To prevent malaria, you must do everything possible to avoid mosquito bites. You should advise everyone in your community to act together to:
- Get rid of standing water where mosquitoes breed; drain pits that fill with rain water; cover or get rid of tin cans and pots that collect water near the house.
- Stay away from spending the night in wet places where mosquitoes breed.
- Use bed nets treated with insecticide, a mosquito-killing chemical. In many parts of Ethiopia you are able to distribute insecticide treated nets (ITNs; see Figure 18.4) to families who need them. These nets protect people who sleep under them from being bitten by mosquitoes, and they also reduce the risk to others sleeping in the same room because the insecticide repels mosquitoes from entering the house.

Preventing malaria should be an individual and a community responsibility. Consider holding a health campaign aimed at raising awareness of how to prevent malaria, using the health promotion techniques you learned about in Study Session 2 of this Module. Make sure the pregnant women you see for antenatal care know that they, their unborn baby and their children under 5 years are all at increased risk of malaria.
Learning Outcomes for Study Session 18
