If you have been working with children for some time, or if you are familiar with mental health services for adults, you may have heard the word CAHMS used in relation to service provision. In most areas of the UK, Child and adolescent mental health services (CAMHS) are commissioned to work with children and young people up to the age of 18 who are experiencing emotional or mental health problems. It is not possible for a young person or their parents to self-refer, and there are a number of reasons for this. One of the main being that professionals working in primary care and schools, such as GPs, school doctors and nurses, educational psychologists, special educational needs coordinators and social workers are often best placed to provide initial help. They tend to be based in the young person’s community and can draw on their professional networks to organise support around the needs of the young person and their family. CAMHS take over when the practitioners with more generalist skills identify the need for specialist care, e.g. prescribing medication, advanced therapy skills and specialist skills aligned to particular mental health issues. These practitioners based in local communities are essentially the ‘gatekeepers’ for the more specialist CAMHS.
CAMHS is typically represented by a tier structure. Tier 1 represents ‘universal’ services with a remit to promote good mental health. Tier 2 represents more targeted services that can support young people with the less severe problems. Tier 3 is the beginning of the specialist services that deal with more severe needs, usually on an outpatient arrangement. Tier 4 is highly specialist and often involves a hospital stay (ACAMH, 2020). Click through the tabs to read an explanation of each of the tiers.
Active content not displayed. This content requires JavaScript to be enabled.
Interactive Figure 4: The CAMHS four tier structure
Show description|Hide descriptionA rectangular box with four clickable tabs, explaining the four tiers of CAMHS:
Tier 1: Universal services, such as primary care, including general medical practice, school nursing, health visiting and schools. Tier one services aim to promote mental well-being.
Tier 2: More targeted services, such as youth offending teams, primary mental health workers, and school and youth counselling (including social care and education). This includes support for children with less severe mental health problems.
Tier 3: Specialist community CAMHS. These are multi-disciplinary teams of child and adolescent mental health professionals providing a range of interventions, including teams with specific remits, such as CAMHS learning disability teams; community forensic CAMHS; adolescent substance misuse teams; crisis/home treatment teams preventing admission to hospital; liaison teams providing CAMHS input to children and young people in acute care settings.
Tier 4: Highly specialist services, such as day and inpatient services. Very specialised outpatient services, and, increasingly, services such as crisis/home treatment services which provide an alternative to admission. These are generally services for a small number of children and young prople who are deemed to be at greatest risk of rapidly declining mental health, or from serious self-harm, who need a period of intensive input.
Interactive feature not available in single page view (
see it in standard view).
Revisiting the ‘mental health spectrum’ introduced in Session 2 and considered again in Session 6, a young person would need to be ‘struggling’ and moving into the ‘unwell’ zone for a referral to specialist services.

Figure 5: Mental health spectrum (repeated from Session 2.) Show description|Hide descriptionA diagram of an arrow, on the left it is green with the word ‘healthy’, then it changes to yellow with the word ‘coping’. Then it moves to red with the word ‘struggling’, then it moves to a dark red, with the word ‘unwell’.
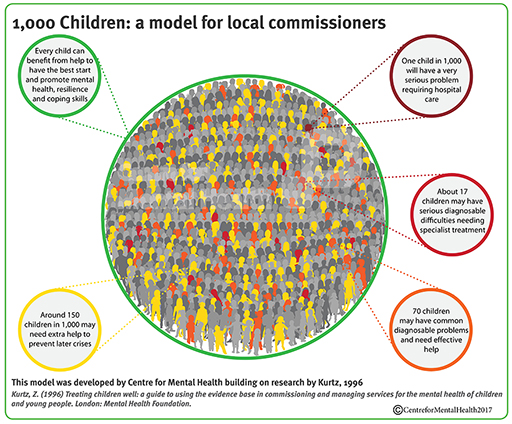
To put things into perspective, look at this infographic developed by the Centre for Mental Health (2017). Based on 1996 research, the figures will not be quite up to date. They do, however, provide a sense of proportion, based on a population of 1000 children and young people, about the levels of support likely to be needed at any one time.
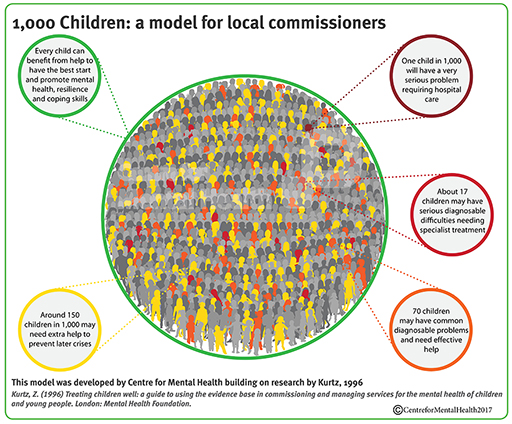
Figure 6: 1,000 children: a model for local commissioners
Show description|Hide descriptionAn illustration demonstrating statistics for 1,000 children: a model for local commissioners. In the centre is a circle full of outlines of people. There are five circles coming from the middle and surrounding the main image. From the top left, going clockwise: ‘Every child can benefit from help to have the best start and promote mental health, resilience an coping skills.’ ‘One child in 1,000 will have a very serious problem requiring hospital care.’ ‘About 17 children may have serious diagnosable difficulties needing specialist treatment.’ ‘70 children may have common diagnosable problems and need effective help.’ ‘Around 150 children in 1,000 may need extra help to prevent later crises.’ At the bottom of this, there is the following text: This model was developed by Centre for Mental Health building on research by Kurtz, 1996. Kurtz, K. (1996) Treating children well: a guide to using the evidence base in commissioning and managing services for the mental health of children and young people. London: Mental Health Foundation. © Centre for Mental Health 2017
As this infographic highlights, at any one time, out of 1000 children and young people:
- about 150 have a high risk of poor mental health and may need extra help to prevent later problems;
- a further 70 will have a common diagnosable problem for which they need effective help;
- 17 will have a serious problem needing specialist treatment;
- one will have a very serious condition that requires hospital care.
It also illustrates the complexity of mental health and the importance of exploring the referral process in order to receive the most appropriate support and treatment. You will explore this next.