Using wellbeing indicators
You may be familiar with the wellbeing indicators outlined by the policy ‘Getting it Right for Every Child’ (GIRFEC). You can read more about these online here:
Getting it Right for Every Child [Tip: hold Ctrl and click a link to open it in a new tab. (Hide tip)]
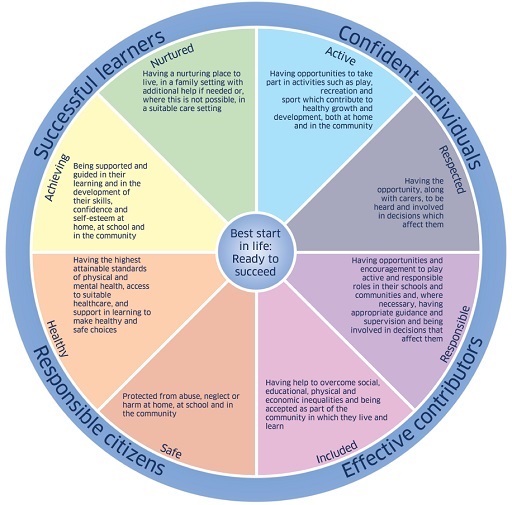
GIRFEC includes wellbeing indicators, illustrated in Figure 4.4. These indicators can help you think about the different influences on a child’s wellbeing and help you think about how you might need to support a child or involve other professionals. You might find it helpful to have a list of the wellbeing indicators to hand while you complete Activity 4.3.
Activity 4.3 Using observations and communication to support a health concern
This activity asks you to think about the help Arianna might need for her eyesight, and about how you would ensure this help is sought.
Read the following scenario, then choose which option you think is the best approach to take.
Arianna, who is three, is very adept at using her whole body to explore an environment. She often climbs and rolls on surfaces, both indoors and outside. You have noticed that she has bumped into other children a few times recently and seems more physically cautious than usual. Arianna seems to be taking more time to approach new physical challenges.
You wonder if this is because Arianna is growing and is adapting to her longer limbs. You have noticed other children having to learn how to coordinate their changing body. However, you have noticed that Arianna’s eyes sometimes move independently, with one eye focusing inwards. You wonder whether Arianna’s vision is affecting her movement. You discuss this with a colleague, who thinks that Arianna might have a squint and should see an optician. You don’t know whether Arianna’s parents have noticed, and you decide to speak to them.
- When do you think would be the best time to speak to Arianna’s parents?
a.At the beginning of the day or at the end-of-day pick-up.
Comment
Parents (and staff) will be busy and have their own agenda, such as catching a bus or getting to work. They may not be in a frame of mind to discuss a sensitive issue. Conversations will be public if you are in the main space. All children will be present and may be listening in to a sensitive issue. However, you could use this contact time to ask for a conversation. Perhaps you could ask when it would be a good time to call?
b.At a specific pre-agreed time during the day.
Comment
You could agree a specific time to speak in advance by phone call, a quick chat at pick up or by email. You could discuss the matter on the phone but agree a time to call. A parent should have the opportunity to ensure they are in a private space to discuss their child on the phone and if you are calling them at work this might not be possible.
Where do you think you should have a conversation?
- a.In a corridor or the main nursery space.
Comment
These are public spaces and not confidential. Other children and adults will be listening. This is not private or dignified, and there is also likely to be noise and distraction.
b.In a private room.
Comment
This is preferable, and better still with the chance to make a cup of tea. Try to create a friendly family room that hosts positive experiences as well as potentially difficult conversations. Think about the layout and decoration. You’d like to create a calm, positive and welcoming atmosphere in the space you create before you even start to talk. You could speak on the phone, but you need to be in a private room to do this too.
How might you prepare for this conversation?
Comment
Review the wellbeing indicators above and makes some notes in your reflective journal about what kind of information you might need and how you might raise your concerns. You might consider the comments in Section 4.2 and the importance of neutrality in your approach. You may need to consider whether the parent has communication needs.
What did you decide?
Discussion
Perhaps you considered these points?
You might refer to your notes on observing Arianna’s physical confidence and her enjoyment of exploring her space with her whole body. The context for your observation is your understanding of her enthusiasm and confidence in physical activity.
Look up information about eyesight and the importance of intervening early. Don’t presume to diagnose a squint, but have information available about the importance of eye checks.
Start by talking about what you and parents both know about Arianna’s physical abilities and coordination, and then share your concern that her eyesight might be hindering her.
Focus on Arianna’s capabilities. You may have noticed that she is finding ways to manage the challenges of her eyesight, perhaps taking longer to assess how to move about in a space. Arianna is adapting to the challenge she is facing so she may not be upset or even really notice what is different. You do not know what will be revealed through an eye check, but you can help focus on Arianna’s competence and active learning, which will support her and her parents through diagnosis of any medical condition.
Share the information you have found about eyesight, stressing that you are not the expert but that she might need support for her vision now. Make suggestions for action such as visiting an optician, GP or health visitor.
Follow up the conversation and ask parents to let you know what the outcome is and find out if there is any action you might need to take. Remember if parents do not follow up on your suggestion of getting a professional’s opinion, you may need to talk to the child’s health visitor about the need for an eye check. Before doing so it will be important to check guidelines on information-sharing when there is a welfare concern (as opposed to a child protection concern), then parental permission will be needed to discuss this with a health visitor.
If you need to share information with another professional, such as a health visitor, practitioners should take families’ views into account and be clear about:
– what information they propose to share to support wellbeing
– who it will be shared with and why.
Families have no obligation to accept help offered to support wellbeing. However, if a child is considered to be at risk of significant harm, then information may be shared without consent and immediately.
Assessing Arianna’s wellbeing
A practitioner concerned about a child’s eye health is already using the health wellbeing indicator. They might also consider Arianna’s more cautious approach to being active and be aware of the potential for a loss of confidence as she struggles to take on physical challenges that were previously easy for her. This means considering the ‘Active’ and ‘Achieving’ wellbeing indicators.
The practitioner respects Arianna’s experience and her approach, and notices not just the difficulties that Arianna is experiencing, but also how she manages to deal with them and how she is flexible and thoughtful in adapting her body.

Arianna may need support with her eyesight, and it is important that this is addressed. It is important to draw attention to the way that Arianna manages to deal with her challenging eyesight and find new ways to assess risk or perceive distance. What will be helpful is discussing the issue with Arianna herself so that she feels respected, another wellbeing indicator. Arianna is a unique, competent and active learner, not a child with an eye problem.
The example of the concern about Arianna’s eyesight provides you with an approach that you might find helpful when faced with other concerns.
The following section explores ways that you can build a community of support to help you and colleagues in your setting to work effectively together for children with ASN.
What you focus on is what grows