1.5 General danger signs (GDS)
Since IMNCI takes a holistic approach to assessing, classifying and treating childhood illnesses it is important to look for general danger signs as well as symptoms and signs of specific childhood illnesses.
The general danger signs are signs of serious illness that are seen in children aged two months up to five years and will need immediate action to save the life of the child. There are five general danger signs and these are set out in Box 1.2 below (reproduced from the IMNCI Assess and Classify Chart Booklet, FMOH Ethiopia, June 2008). Make sure that any infant or child with any danger sign is referred after receiving urgent pre-referral treatment.
Box 1.2 Checking for general danger signs
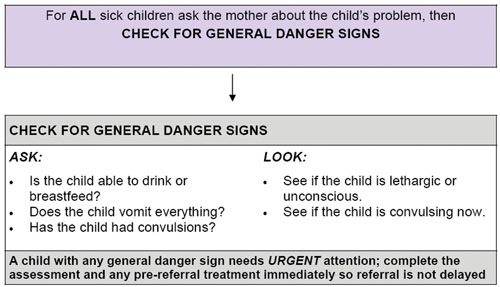
As you can see in Box 1.2, there are key questions you need to ask and signs you need to look for.
![]() You should assess all sick children who come to your health post for general danger signs. Most children with a general danger sign need urgent referral to hospital.
You should assess all sick children who come to your health post for general danger signs. Most children with a general danger sign need urgent referral to hospital.
A child with a general danger sign has a serious problem. Most children with a general danger sign need urgent referral to hospital. They may need lifesaving treatment with injectable antibiotics, oxygen or other treatments that may not be available in the health post. You should complete the rest of the assessment immediately and give urgent pre-referral treatments before sending the patient to the next facility. You will learn more about this later in this study session.
You are first going to look in more detail how you check for general danger signs.
ASK: Is the child able to drink or breastfeed?
A child has the sign ‘not able to drink or breastfeed’ if the child is not able to suck or swallow when offered a drink or breastmilk.
When you ask the mother if the child is able to drink, make sure that she understands the question. If the mother replies that the child is not able to drink or breastfeed, ask her to describe what happens when she offers the child something to drink. For example, is the child able to take fluid into his mouth and swallow it?
If you are not sure about the mother’s answer, ask her to offer the child breastmilk or a drink of clean water. Look to see if the child is swallowing the breastmilk or water.
A child who is breastfed may have difficulty sucking when his nose is blocked. If the child’s nose is blocked, clear it. If the child can breastfeed after the nose is cleared, the child does not have the danger sign, ‘not able to drink or breastfeed’.
ASK: Does the child vomit everything?
A child who is not able to hold anything down at all has the sign ‘vomits everything’. A child who vomits everything will not be able to hold down food, fluids or oral drugs. A child who vomits several times but can hold down some fluids does not have this general danger sign.
When you ask the question, use words the mother understands. Give her time to answer. If the mother is not sure if the child is vomiting everything, help her to make her answer clear. For example, ask the mother how often the child vomits. Also ask if each time the child swallows food or fluids, does the child vomit? If you are not sure of the mother’s answers, ask her to offer the child a drink. See if the child vomits.
ASK: Has the child had convulsions?
During a convulsion, the child’s arms and legs stiffen because the muscles are contracting or if the child has repeated abnormal movements. The child may lose consciousness or not be able to respond to spoken directions. Ask the mother if the child has had convulsions during this current illness. Use words the mother understands. For example, the mother may know convulsions as ‘fits’ or ‘spasms’. See also if the child is convulsing now.
LOOK to see if the child is lethargic or unconscious
A lethargic child is not awake and alert when he should be. The child is drowsy and does not show interest in what is happening around him. Often the lethargic child does not look at his mother or watch your face when you talk. The child may stare blankly and appear not to notice what is going on around him. An unconscious child cannot be wakened. He does not respond when he is touched, shaken or spoken to.
Ask the mother if the child seems unusually sleepy or if she cannot wake the child. Look to see if the child wakens when the mother talks or shakes the child or when you clap your hands. However, if the child is sleeping and has cough or signs of difficult breathing, you must count the number of breaths first before you try to wake the child because it is easier to count the exact breathing rate when the child is calm.
When you have completed the above steps, you should record what you have found on the sick child case recording form. You must circle any general danger signs that are found, and check (✓) against the appropriate answer (yes or no) in the classify column. Case study 1.1 below illustrates the assessment process for general danger signs in practice.
Case Study 1.1 Fatuma’s story
Fatuma is 18 months old. She weighs 11.5 kg. Her temperature is 37.5°C. The health worker asked, ‘What are the child’s problems?’ The mother said ‘Fatuma has been coughing for six days, and she is having trouble breathing’. This is the initial visit for this illness.
The health worker checked Fatuma for general danger signs. The mother said that Fatuma was able to drink. She had not been vomiting. She had not had convulsions during this illness. The health worker asked, ‘Does Fatuma seem unusually sleepy?’ The mother said, ‘Yes’. The health worker clapped her hands. She asked the mother to shake the child. Fatuma opened her eyes, but did not look around. The health worker talked to Fatuma, but the child did not watch her face. Fatuma stared blankly and appeared not to notice what was going on around her.
The top part of the sick child case recording form for the above case is reproduced for you in Figure 1.2 below. You can see the relevant information from the case study has been recorded.
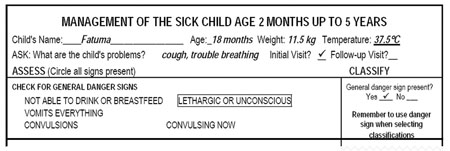
![]() For any child who has a general danger sign you must complete the rest of the assessment process immediately. The presence of a general danger sign indicates a severe classification and the need for urgent referral.
For any child who has a general danger sign you must complete the rest of the assessment process immediately. The presence of a general danger sign indicates a severe classification and the need for urgent referral.
If the child has a general danger sign you should complete the rest of the assessment process immediately. After checking the general danger signs, you should assess the child for cough/difficult breathing, diarrhoea, fever, ear problems, malnutrition, anaemia and HIV. The presence of any one of the general danger signs indicates a severe classification. A child with a general danger sign or a severe classification should be referred immediately to the health centre after giving appropriate pre-referral treatments.
In Case Study 5.1, Fatuma has the general danger sign ‘lethargic or unconscious’ which is a severe problem. You would complete the rest of the IMNCI assessment and refer her urgently after giving the necessary pre-referral treatments for her classifications, including treatment to prevent low blood sugar. Since she is able to feed, you would ask the mother to breastfeed Fatuma or give her a coffee cup of milk or sugar-water solution. You will learn about the pre-referral treatments in the subsequent study sessions in this Module.
What action should you take if a child has one or more of the general danger signs?
From the materials you have read so far, you know that if a child has any one of the five general danger signs, that child must be considered seriously ill and therefore you should make an immediate referral to a health centre.
This study session has introduced you to the IMNCI case management process and outlined the importance of this in helping to reduce death, illness and disability for babies and children in your community. You have seen that you have an important role to play in this respect. The remaining study sessions in this module will explain to you how to assess and treat children and young infants with a range of conditions, including:
- cough/difficult breathing, diarrhoea, fever, ear problems, malnutrition and anemia, HIV, immunization status and other problems (all sick children)
- serious bacterial infection, diarrhoea, HIV infection, feeding problems or low weight, immunization status and other problems (young infants).
1.4.1 The IMNCI case management process
