5.2 Assess diarrhoea in children
All sick children that come to your health post should be checked for diarrhoea.
ASK: Does the child have diarrhoea?
- If the mother answers no, ask about the next main symptom, fever. You do not need to assess the child further for signs related to diarrhoea.
- If the mother answers yes, or if the mother said earlier that diarrhoea was the reason for coming to the health post, record her answer. Then assess the child for signs of dehydration, persistent diarrhoea and dysentery.
You need to assess the following:
- How long the child has had diarrhoea
- Whether there is blood in the stool to determine if the child has dysentery, and
- Any signs of dehydration.
Box 5.1 sets out the signs you need to ask about and look for when assessing a child who has diarrhoea.
Box 5.1 Assessing diarrhoea in a child
| Does the child have diarrhoea? IF YES ASK: | LOOK AND FEEL |
|---|---|
● For how long? ● Is there blood in the stool? | ● Look at the child’s general condition. Is the child: - Lethargic or unconscious? - Restless and irritable? - Look for sunken eyes. ● Offer the child fluid. Is the child: - Not able to drink or drinking poorly? - Drinking eagerly, thirsty? ● Pinch the skin of the abdomen. Does it go back: - Very slowly (longer than two seconds)? - Slowly? |
You will now look at the steps for assessing diarrhoea in a child in more detail.
ASK: For how long has the child had diarrhoea?
- Give the mother time to answer the question. She may need time to recall the exact number of days.
ASK: Is there blood in the stool?
- Ask the mother if she has seen blood in the stools at any time during this episode of diarrhoea.
Next, you need to check the child for signs of dehydration.
A child who becomes dehydrated is at first restless and irritable. If dehydration continues, the child becomes lethargic or unconscious. As the child’s body loses fluids, the eyes may look sunken. When pinched, the skin will go back slowly or very slowly. To assess whether the child is dehydrated, and how seriously, you need to look and feel for the following signs.
LOOK at the child's general condition
LOOK to see if the child is lethargic or unconscious. Or, is the child restless and irritable?
When you checked for general danger signs, you checked to see if the child was lethargic or unconscious. If the child is lethargic or unconscious, he has a general danger sign. Remember to use this general danger sign when you classify and record the child’s diarrhoea.
![]() If a child is lethargic or unconscious this is a general danger sign.
If a child is lethargic or unconscious this is a general danger sign.
The sign restless and irritable is present if the child is restless and irritable all the time or every time he is touched and handled. If an infant or child is calm when breastfeeding, but again becomes restless and irritable when breastfeeding stops, he has the sign ‘restless and irritable’. However, many children are upset just because they are in the health post and in unfamiliar surroundings. Usually these children can be consoled and calmed. They do not have the sign ‘restless and irritable’.
LOOK for sunken eyes
- The eyes of a child who is dehydrated may look sunken. Decide if you think the eyes are sunken. Then ask the mother if she thinks her child’s eyes look unusual. Her opinion helps you confirm whether the child’s eyes are sunken.
- You should note that in a severely malnourished child who is visibly wasted, the eyes may always look sunken, even if the child is not dehydrated. However, although sunken eyes is less reliable in a visibly wasted child, you should still use the sign to classify the child’s dehydration.
OFFER the child fluid. Is the child not able to drink or drinking poorly? Or, is the child drinking eagerly, thirsty?
- Ask the mother to offer the child some water in a cup or spoon. Watch the child drink. A child is not able to drink if he is not able to suck or swallow when offered a drink. A child may not be able to drink because he is lethargic or unconscious.
- A child is drinking poorly if the child is weak and cannot drink without help. He may be able to swallow only if fluid is put in his mouth.
- A child has the sign drinking eagerly, or thirsty if it is clear that the child wants to drink. Look to see if the child reaches out for the cup or spoon when you offer him water. When the water is taken away, see if the child is unhappy because he wants to drink more.
- If the child takes a drink only with encouragement and does not want to drink more, or refuses to drink, he does not have the sign ‘drinking eagerly, thirsty’.
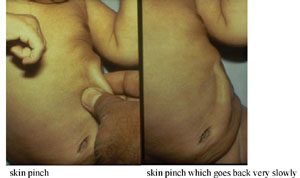
PINCH the skin of the abdomen. Does it go back very slowly (longer than two seconds) or slowly?
- Ask the mother to place the child on the examining table so that the child is flat on his back with his arms at his sides (not over his head) and his legs straight. Or, ask the mother to hold the child so he is lying flat on her lap. Locate the area on the child’s abdomen halfway between the umbilicus and the side of the abdomen. To do the skin pinch, use your thumb and first finger. Do not use your fingertips because this will cause pain. Place your hand so that when you pinch the skin, the fold of skin will be in a line up and down the child’s body and not across the child’s body. Firmly pick up all of the layers of skin and the tissue under them. Pinch the skin for one second and then release it. If the skin stays up for even a brief time after you release it, decide that the skin pinch goes back slowly.
- When you release the skin, look to see if the skin pinch goes back:
- very slowly (longer than two seconds)
- slowly
- immediately.
The photographs in Figure 5.1 show you how to do the skin pinch test and what the child’s skin looks like when the skin pinch does not go back immediately.
The skin pinch test is not always an accurate sign of dehydration because in a child with severe malnutrition, the skin may go back slowly even if the child is not dehydrated. In an overweight child, or a child with oedema, the skin may go back immediately even if the child is dehydrated. However even though skin pinch is less reliable in these children, you should still use it to classify the child's dehydration.
What are the possible assessments you might make for a child with diarrhoea?
You might assess the child for dehydration. If the child has had diarrhoea for 14 days or longer you would assess persistent diarrhoea, and if you see blood in the stool or if the mother tells you that there has been blood in the stool, you would record that the child might have dysentery.
How can you assess whether a child has dehydration?
If the child is irritable and restless, not able to drink or drinks poorly, these are all signs of dehydration. Another sign is a skin pinch that returns slowly or very slowly. You should also remember that if a child is lethargic or unconscious this is one of the general danger signs as well as a possible sign of dehydration.
Following your assessment of the child for diarrhoea and dehydration, your next step is to classify the diarrhoea. How you do this will depend on the age of the child, and you are going to look at this next.
5.1 Assess and classify diarrhoea
