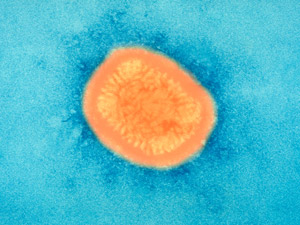
 Electron microscope image of smallpox virus
Human history can be written alongside a history of human infectious disease. Pathogens, or organisms that cause disease, need us in order to reproduce, so they evolve with the species they infect and upon which they depend.
Electron microscope image of smallpox virus
Human history can be written alongside a history of human infectious disease. Pathogens, or organisms that cause disease, need us in order to reproduce, so they evolve with the species they infect and upon which they depend.
Microbial pathogens include bacteria, viruses, fungi and tiny parasitic animals. Although typically very small, pathogens pack a weighty punch in their tiny innards. In fact, the smallpox virus is 300 times smaller than the width of a human hair, not bad for an organism that may be responsible for more deaths than any other pathogen in human history.
Smallpox has been a lethal killer for millennia, with its known history stretching back at least 10,000 years. It was not selective in who it killed, from peasant to Pharoah, with Ramesses V of Egypt being a notable victim. But after a highly successful global vaccination campaign, the last naturally occurring case of smallpox was declared on 26 October 1977.
The health authorities must have been optimistic that eradication of other human diseases would follow. For instance, another ancient disease, tuberculosis (TB), was thought to be on the road to elimination just a few short decades ago. But its resurgence means that it is now believed to infect about a third of the world’s population.
This doesn’t mean that two billion people have active TB, but that the TB bacterium lurks within their cells, waiting for its moment to attack when the immune system is weak.
And unfortunately, TB has taken advantage of infection with another pathogen: HIV – the virus that causes AIDS. One consequence of HIV is that it supresses the immune system.
If an individual infected with HIV has dormant TB, then often active tuberculosis will follow; this co-infection has been a major reason why TB has taken hold and become much more difficult to treat.
Progress has been made in treating other major infections. A scourge of Europe from the late 15th century on was the sexually transmitted disease syphilis, caused by a corkscrew-shaped bacterium.
It is possible that it was brought to Europe by the ships of Columbus returning from the New World, although this cannot be proven. It occurred in three stages, starting with a localised skin lesion that would then clear up.
Further symptoms occurred with latent periods in between until sometimes several decades later, tertiary syphilis arrived. This can lead to paralysis, blindness, dementia and eventually death.
Some have even suggested that Henry VIII’s growing megalomania and inability to produce many viable offspring, despite an abundance of wives and mistresses, were due to syphilis infection.
Fortunately, syphilis is now readily treatable with antibiotics. But what if we didn’t have antibiotics? This might seem fanciful now; most of us can’t remember when we didn’t routinely have these wonder drugs to treat what seem like trivial infections.
But it was not so long since the first patient, Albert Alexander, was treated for a nasty infection caused by a rose thorn – 1941 in fact. An injection with the antibiotic penicillin immediately had a dramatic effect on the infection, causing it to retreat.
The doctors had insufficient drugs to get rid of it altogether, so sadly, Albert died. This first treatment led to the start of the antibiotic era, which we now take for granted.
But what if the antibiotics stop working? Alarmingly, this is starting to happen. Many bacteria are becoming resistant to some antibiotics, and a few seem to be resistant to virtually all antibiotics.
Although very small and apparently simple, bacteria have some powerful tools at their disposal and one is the ability to transfer genes for antibiotic resistance to other bacteria. So if one strain becomes antibiotic-resistant, others will follow. And then we would be back to where we were before 1941, which isn’t a pleasant prospect.
There are some good news in our battle with one high-profile virus; treatment for HIV is now so effective that most infected people can live a normal life. Of course, we have yet to find a way to readily treat most viral infections, as shown by the Covid-19 pandemic. Doctors can treat the symptoms but not the virus itself and at the time of writing, there is no vaccine for Covid-19.
So in the battle between humanity and nature, nature seems to retain the upper hand. We need to work hard to keep up and continue to develop new ways of dealing with infectious agents because you can be sure there are more pathogens out there, waiting for their moment to come.
Rate and Review
Rate this article
Review this article
Log into OpenLearn to leave reviews and join in the conversation.
Article reviews