3.2 Interferons and anti-viral proteins
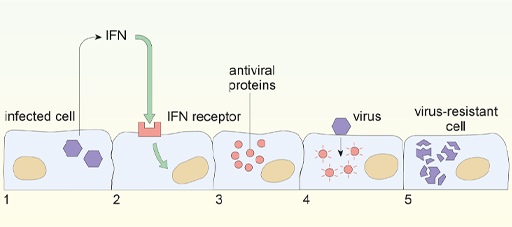
When cells become infected, interferon (IFN) signals to neighbouring cells to induce synthesis of anti-viral proteins, which are normally inactive, but it puts the cell into a state of ‘alert’. Should the neighbouring cells later become infected, viral components activate the antiviral proteins, to shut down mRNA production and protein synthesis. This process is shown diagrammatically in Figure 10. An infected cell (1) releases IFN, which acts on receptors on neighbouring cells (2) to induce antiviral proteins (3). If that cell later becomes infected with a virus, the antiviral proteins are activated (4) to induce a virus-resistant state where protein synthesis is inhibited (5).
-
What advantage is there for a cell to shut down protein synthesis? What advantage is there for the infected host?
-
There is no advantage to the individual cell, since all cells must synthesise protein to survive, however it also stops virus production in that cell and thus slows virus spread within the body.
Interferons were originally identified for their role in limiting virus replication. However, they have numerous additional effects in the adaptive immune system. Specifically, they enhance the ability of all cells to present antigens to T lymphocytes (T cells), which are primarily responsible for elimination of virus-infected cells. You will hear a lot more about this in Week 2. But first we look at one more element of the innate immune system: how a replicating virus is detected.