3.4 Adapting vaccines
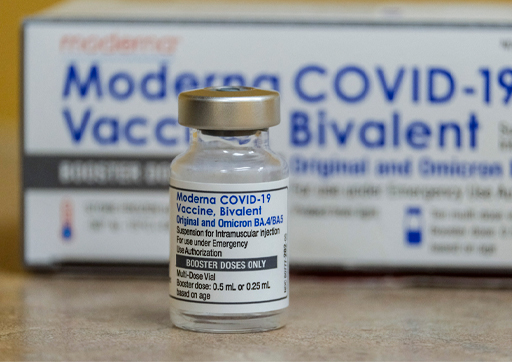
The majority of the COVID-19 vaccines are designed to induce an immune response against the spike protein. The mRNA vaccines have been particularly successful in this regard. Moreover, it is possible to modify an mRNA vaccine quite quickly; the gene sequence encoding the spike protein of any new variant can be rapidly identified and the new sequence is then used in the vaccine. This approach has been taken by both Pfizer/Biontech and Moderna. In January and February 2022 both companies produced a ‘bivalent vaccine’ which included both mRNA of the original spike protein and mRNA for the omicron BA.1 spike protein. These formulations were approved in the UK in August 2022 and used in the Autumn booster programme that year. Additional bivalent vaccines have since been developed (Figure 8).
New formulations are screened for safety and monitored in use to see whether they produce more adverse reactions than the original vaccine.
The vector vaccines against spike protein can also be modified relatively quickly, by inserting a gene for the new sequence into the vector. Vector vaccines have some advantages in that they are cheaper to produce and require a simpler cold-chain than mRNA vaccines. However, there is the possibility that an immune response will be produced against components of the vector itself, which means that successive boosts with a vector vaccine become less effective.
Production of a variant spike protein, to use in a component vaccine is certainly possible, but likely to be more complicated and time-consuming than modifying an mRNA or vector vaccine.
Finally, one must not neglect the potential use of inactivated virus vaccines. Although these were the last to come through the development process during the COVID-19 pandemic, they do have one potential advantage. Since they include all the protein components of the virus (including the core structural proteins that mutate less) they may be more effective at producing cross-strain immune responses.
An important final consideration is not just how quickly a variant-specific vaccine can be made in the laboratory, but also how long it takes to scale-up production. Clearly no-one wants to commit to the production of large quantities of vaccine unless it is genuinely necessary. For future years we can anticipate that new COVID-19 booster vaccines will be produced and given selectively to more vulnerable groups, much as influenza-A vaccines have in the past.
