2 How antibiotic resistance spreads
In Week 4, you learned that, in the presence of antibiotics, resistant bacteria have a survival advantage over sensitive bacteria and can quickly dominate a bacterial population. Resistance is an inevitable consequence of using antibiotics. The more that antibiotics are used, the more widespread resistance becomes.
You have also learned that antibiotic resistance spreads in a bacterial population by resistance genes passing from one bacterium to another. In Activity 2, you will discover that antibiotic resistance also spreads when resistant bacteria move from one human or animal host to another.
Activity 2 How does antibiotic resistance spread?
First, watch the video below which shows how antibiotic resistance spreads in different communities.

Transcript: Video 2 How does antibiotic resistance spread?
Now, answer the following questions:
- In which ways can people be infected by antibiotic-resistant bacteria?
- What roles do people moving from one geographical region to another play in spreading antibiotic resistance?
Answer
- Antibiotic-resistant bacteria can spread to humans through food and through direct contact with animals or other people (for example, via unclean hands or contaminated objects). Resistance may also develop naturally if a person takes antibiotics to treat a bacterial infection. You will learn more about how infections are spread between people in Week 7.
- The numbers of people travelling abroad for work or holidays is rising. This increases the likelihood that resistant bacteria, acquired from food or the environment, will be brought home and spread to other people.
Antibiotics eventually end up in the environment. Contaminated soil and waterways become reservoirs of antibiotics and antibiotic-resistant bacteria. This creates
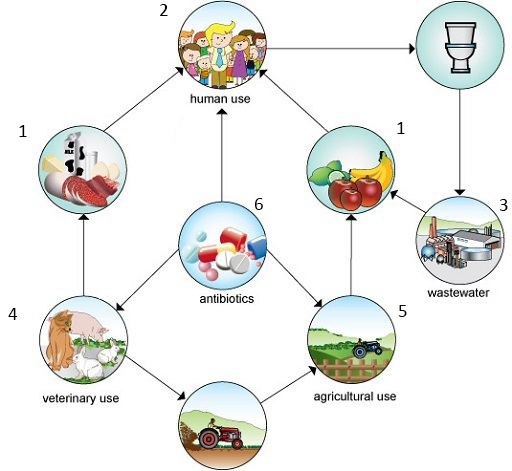
Two interrelated factors contribute to the spread of antibiotic resistance. An increased rate of resistance, which results in higher numbers of antibiotic-resistant bacteria, and a greater number of cases of infectious diseases. Both factors increase the use of antibiotics which, in turn, drives the antibiotic resistance rate.
In the following sections, you will look at the main drivers of antibiotic resistance:
- poor hygiene and infection control
- the overuse of antibiotics
- the misuse of antibiotics.
You will also consider how the lack of new antibiotics and gaps in global infection and resistance data exacerbate the problem.
