1.3 What are the consequences of falls?
Falls are devastating. They have a direct impact on the person affected, their family and caregivers, as well as incurring considerable economic cost.
A quarter of all falls result in injury. Injuries range from soft tissue injuries, through to fractures and head injuries that require hospitalisation. Even before Parkinson’s has been diagnosed the risk of sustaining a fracture and traumatic brain injury is increased compared to those without Parkinson’s (Camacho-Soto et al, 2017). This may suggest that there are sub-clinical motor and non-motor features present that contribute to this risk.
People with Parkinson’s are at higher risk of experiencing traumatic brain injury following a fall. Fracture risk is doubled in Parkinson’s with a tripled risk of hip fracture (Pouwels et al, 2013). Once a hip fracture has occurred, people with Parkinson’s are at higher risk of sustaining a second hip fracture (Harvey 2018). Vertebral fractures are also common but the associated stooped posture may be wrongly attributed to Parkinson’s alone (Torsney et al, 2014). Hip fractures are sustained more commonly than wrist fractures as people with Parkinson’s tend to fall ‘like a log’ with their arms adducted to their sides (Carpenter et al, 2004). In recent years, hip fractures have accounted for 4% of all emergency admissions in Parkinson’s and for 7.6% of admission costs (£13 million per annum for England and Wales in 2014) (Low et al, 2015).
Hip fractures may have grave consequences, with only half of patients returning to their previous level of function (Holt et al, 2008). Even when we take into account poorer pre-fracture mobility, the consequences of hip fractures for people with Parkinson’s are worse than among the general population. This is because they experience higher pressure sore rates, a more than doubled length of stay in hospital and a greater proportion of bed/wheelchair dependency after 30 days (Walker et al, 2013). Parkinson’s-specific institutionalisation and mortality rates after hip fracture are unknown but are likely greater than the general population.
As a result of falling, many people with Parkinson’s develop ‘fear of falling’. This concept encompasses concerns about falling and loss of balance confidence: It also includes low fall-related efficacy, which is someone’s confidence or belief in their ability to perform activities without losing balance or falling. This can lead to activity avoidance. In turn, people who are fearful of falling restrict their social activities and limit their daily activity. This results in loss of independence and isolation, which in turn contributes to immobilisation and perpetuates a cycle of deterioration.
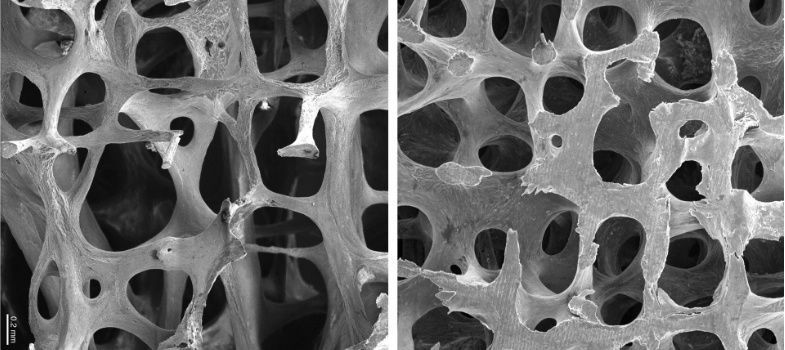
Falls tend to occur in parallel with the emergence of other debilitating, difficult-to-treat features of the condition. This includes dysphagia and cognitive impairment. These features, along with fear of falling, contribute to a state in which people suffer the consequences of immobility. This includes pressure sores, constipation, deconditioning, osteoporosis, inactivity and loss of independence, which in turn contribute to a vicious cycle that further increases the risk of falls.
This section has illustrated the dangers of falls. The next section will look at how to reduce falls risk.
1.2 Why do people with Parkinson’s fall?