4.2.2 Vitamin D
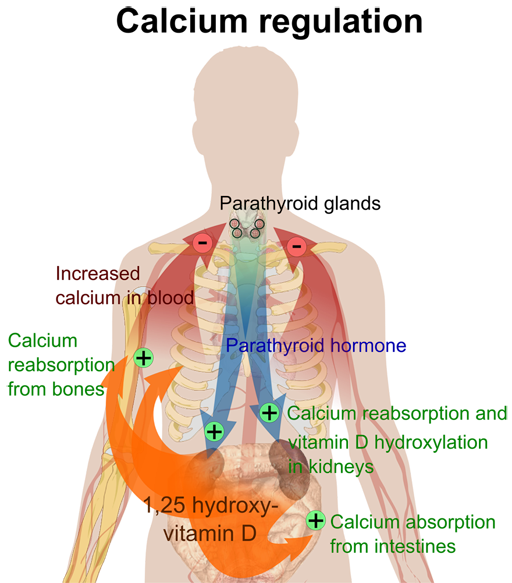
Vitamin D helps regulate calcium handling and plays an essential part in the health of bones, muscles and teeth. For healthy adults in the UK, most vitamin D (~90%) is obtained by the exposure of sunlight to the skin. The sun’s ultraviolet light makes a relatively inactive form of vitamin D (cholecalciferol/vitamin D3) which is converted into an active form of vitamin D principally by the kidneys. The unactived form can also be obtained through diet (but doses are relatively small) or may be supplemented. The ROS leaflet ‘Nutrition for bones’ [Tip: hold Ctrl and click a link to open it in a new tab. (Hide tip)] has more information.
People with reduced sunlight exposure are at risk of vitamin D deficiency, which is common in the UK. Government guidance has recently increased the list of people recommended for supplementation (see ROS website or direct to SACN report).
It is good practice to offer vitamin D supplementation, without the need for testing levels. However, testing may remain appropriate in some people, for example:
- where a patient is reluctant to take supplements, unless deficiency is demonstrated
- where supplements are prescribed but there are concerns about compliance
- where more potent anti-resorptive drug treatments such as Denosumab or i.v. Zoledronic Acid are planned. In these cases, vitamin D must be checked and if necessary replaced before starting treatment
Does the patient require vitamin D maintenance or replacement therapy?
Vitamin D insufficiency is common in Parkinson’s and most patients are not on adequate replacement (Luthra et al, 2018). For most people with Parkinson’s, vitamin D supplementation, to maintain vitamin D levels, will take the form of oral medication containing 800iu of cholecalciferol (vitamin D3) daily. This may or may not be in combination with calcium. Many different forms of such medication exist (soluble/chewable/tablets) and it is usually possible to find one which suits the patient.
Such maintenance treatment may slowly correct low vitamin D levels, although usually higher dose replacement is needed to correct vitamin D deficiency. Where vitamin D is known to be low, and particularly if a potent ‘anti-resorptive’ medication is to be prescribed (see below) then replacement is required more rapidly. It is sensible to ask GPs to check calcium levels in the blood one month after starting treatment. This is because in rare cases an underlying condition called primary hyperparathyroidism can be revealed by the correction of low vitamin D levels. For this same reason, don’t replace vitamin D if the calcium level is high – specialist advice should be sought in this rare scenario.
An example of an appropriate vitamin D replacement schedule is shown below:
| Treatment | Example regime | |
|---|---|---|
Deficiency | 300,000 IU then maintenance | 50,000 IU weekly for 6 weeks then 800-1,600 IU/day |
Insufficiency | 150,000 IU then maintenance | 25,000IU weekly for 6 weeks then 800-1,600 IU/day |
Sufficiency (>50nmol/l) | maintenance | 800-1,600 IU/day |
These higher dose supplements are currently licensed as Fultium but other versions are available depending on local prescribing guidance. Calcium levels should be checked one month after starting these replacement schedules. Retesting of vitamin D levels is not needed unless there are concerns about compliance.
4.2.1 Diet