Supported by over 30 organisations, the Ambitions for Palliative and End of Life Care framework was first released in 2015 and relaunched in 2021 for another five years. It outlines six ambitions, illustrated in the image, to improve the care of dying people.

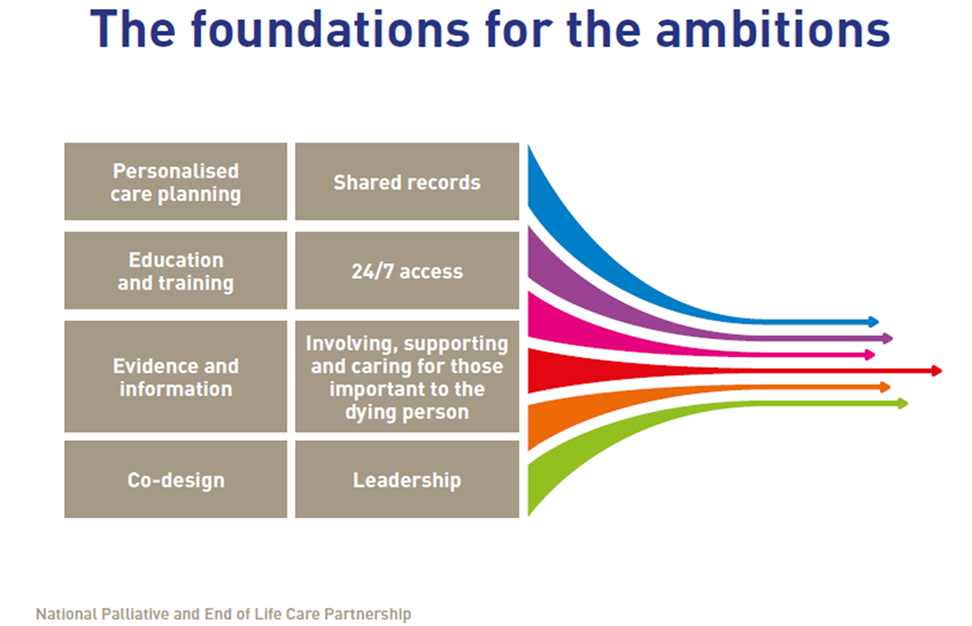
The framework is not mandated health policy. Instead, it serves as guidance for local action to be used by a range of organisations from NHS services, hospices, charities and local authorities. Eight foundations underpin the framework, as outlined in the image below, in order to help people realise the ambitions. These foundations are a combination of infrastructure, actions, and approaches to service design and delivery.
But how do people go from ambition statements to action? How do they go from guidance to changing the care people receive? Researchers have long demonstrated the policy-practice gap and difficulties with implementing guidance in practice (for example, see Borgstrom and Lemos Dekker (2022) for an article about end of life care). In order to examine how people have been using the Ambitions framework, we undertook a multi-modal approach to explore how people understand, interpret, and implement the Ambitions. This approach acknowledges that implementation requires multiple steps that involve making sense of the guidance and accepts that people and organisations may be at different stages of implementation.
In order to examine how people understand the Ambitions framework, we have been talking to them about the language in the document. Here we have heard that people recognise the Ambitions as value statements that reflect ‘good’ palliative and end of life care. People see the Ambitions as providing a ‘shared language’ to talk about care and services. For example, they felt the language in the Ambitions made for useful conversation starters when engaging with partners and commissioners. Yet, they also acknowledge that each Ambition is broad and vague enough to be refined as needed within a service. This enables services to articulate what, for example, coordinated care looks like in their area.
When it comes to examining how people interpret the framework, we have focused on how they relate the framework to what they do – how do they make sense of the Ambitions in relation to their work or experiences? By asking questions about this, we can observe how people make links between the guidance and what they do, which is a step people can take to help them begin to identify how they may implement guidance. For example, in our focus groups and workshops we witnessed how people related the Ambitions to different parts of their work, from patient care to data management and working with others. This step of interpretation helps people make sense of the guidelines for themselves in their role and organisation, moving from ‘what does it mean’ to ‘what does it mean for me’.
Lastly, we looked at how people have implemented the Ambitions. By implementation we mean that they are taking steps to change what they do to align their work more closely with the Ambitions. In our research, we found that services may be implementing the Ambitions in different ways, from focusing on educating staff to larger re-designs of service provision to widen access, or even co-developing community action focused on promoting education and support amongst the population. Importantly for those we spoke to, implementation was not a one-off process but something that involved continuous service redesign, evaluation, and collaboration.
The majority of the people we spoke to were working within palliative and end of life care. Nevertheless, the Ambitions framework is aimed at a much wider audience, and the partnership that created the Ambitions is made up of a wide range of partners. This suggests that there is still much more work to be done if the Ambitions are to be fully realised, to ensure more people become familiar with the guidance and begin their journey of understanding, interpreting, and implementing the framework.
This research was funded by Marie
Curie.




Rate and Review
Rate this article
Review this article
Log into OpenLearn to leave reviews and join in the conversation.
Article reviews