3.2.2 Extended spectrum β-lactamases
In Section 1.2 you saw how β-lactamases can hydrolyse β-lactam antibiotics in order to destroy them. The first β-lactamase to be identified was
In the next activity, you will look at how the presence of ESBLs in E. coli is associated with cephalosporin resistance.
Activity 4 Cephalosporin resistance and ESBLs
The data in this activity are from Pfizer’s antimicrobial testing leadership and surveillance (ATLAS) (Pfizer, 2017).
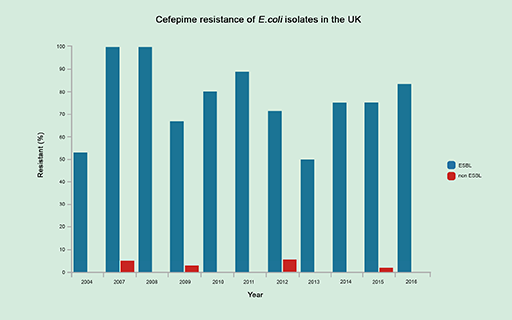
E. coli bacteria were isolated from infections and tested to determine whether they produced ESBLs and whether they were resistant to cephalosporins. Figure 6 shows the percentage of ESBL- and non-ESBL-producing E. coli isolates that were resistant to the cephalosporin cefepime between 2004 and 2016.
Note that this figure compares ESBL-producing and non-ESBL-producing isolates for resistance to cefepime. However, it does not give any information on the number of E. coli isolates that produce ESBLs. As you will see in the case study in Week 4, the percentage of ESBL-producing E. coli isolates in the UK during this period remained below 15% (BSAC UK, 2014).
Now answer the following questions based on the data in Figure 6.
1 How has the proportion of (a) ESBLs and (b) non-ESBLs resistant to cefepime changed over time?
Answer
(a) ESBL-producing E. coli have higher levels of resistance to cefepime than non-ESBL-producing E. coli isolates over the entire period. In 2004, approximately 50% of ESBL isolates were resistant. This increased to a peak of approximately 100% in 2007 and 2008. Resistance decreased between 2008 and 2009 and then rose again until 2011. Resistance reached its lowest level in 2013 before increasing again. Resistance never fell below 50% with the lowest levels in 2004 and 2013.
(b) non-ESBL producing bacteria display hardly any resistance to cefepime with low levels of resistance (less than 10%) only being observed in 2007, 2009, 2012 and 2015.
2 Explain the difference in resistance between ESBL- and non-ESBL-producing E. coli?
Answer
The presence of an ESBL in ESBL-producing E. coli results in the hydrolysis, and therefore destruction, of cefepime. Since cefepime can no longer inhibit PBP, these bacteria are resistant. Non-ESBL-producing E. coli lack the ESBL and cannot hydrolyse cefepime, therefore it can exert its bactericidal effects by binding to and inhibiting its target PBP.
3 Do you think the expression of ESBLs is a major determinant of resistance to cephalosporins in E. coli?
Answer
Resistance to cefepime remains between 50 and 100% in ESBL-producing E. coli whereas almost all non-ESBL-producing bacteria are susceptible to cefepime. This suggests that the presence of an ESBL is a major determinant of cephalosporin resistance.
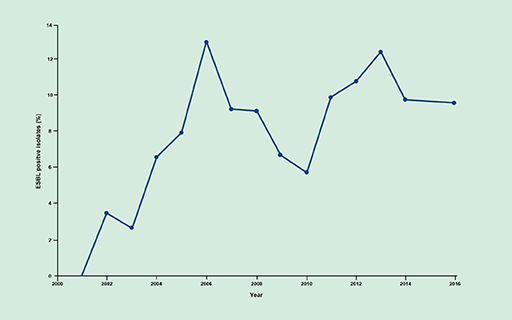
Since they were first described in the early 1980s, the frequency of infections caused by ESBL-producing bacteria has been increasing (Figure 7). Resistance to cephalosporins limits the treatment options for these infections. Consequently, ESBLs represent an ever-growing healthcare challenge.
Several ESBL classes have been identified. Of them, the CTX-M class of ESBLs, has become the most common worldwide. You will learn more about the origin and spread of CTX-M ESBLs in the case study in Week 4.