5.2 Wrong therapeutic use
Antibiotic resistance is more likely to develop when antibiotics are used at too low a dose or taken for too short a time. In the next activity, you will explore the effect of treatment duration on gut bacteria.
Activity 6 Effect of antibiotics on gut bacteria
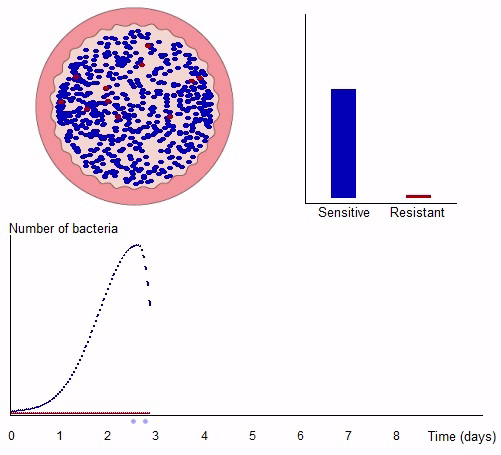
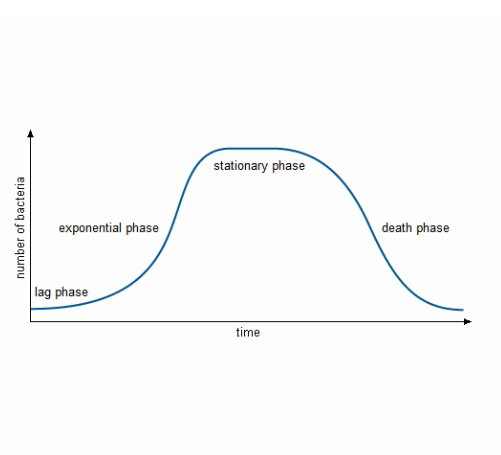
You might recall from Week 1 the typical growth pattern of a bacterial population (Figure 8 below). The death phase does not occur in the gut. This is because of the steady flow of material from mouth to anus, so that new food is always added and waste products are always removed. In the gut, the only time a population will decline like this is if something – for example, an antibiotic taken by mouth – kills it.
When a person swallows pathogenic bacteria, whether they become ill depends on the type of bacterium. For some types, only a few bacteria will cause illness. For other bacteria, millions must be taken in to cause any harm. The number of bacteria needed to cause illness is called the
Now click on the image below to be taken to an interactive activity.
There is a risk of resistance developing every time an antibiotic is used because only resistant bacteria can survive and reproduce in the presence of antibiotics. This process is called
If the dose of antibiotic is too low, selection ensures that a few resistant bacteria will survive. Although the patient may start to feel better, the surviving bacteria will soon multiply, symptoms will return and the antibiotic will no longer be effective at the original dose used.
The concentration of antibiotic within the body decreases with time. Why might failing to take an antibiotic regularly as prescribed make it less effective?
Failure to maintain the antibiotic at a high enough level to kill all the bacteria allows an opportunity for resistant bacteria to be selected and resistance to develop
So far this week you have focused on human behaviours that promote antibiotic resistance. You should by now appreciate the importance of using antibiotics correctly. In the next two sections, you will look at other facets of the problem. First, you will learn why we are running out of options to treat antibiotic-resistant infections.