9.4 Structure of the Ethiopian mental healthcare system
9.4.1 Mental healthcare in Ethiopia
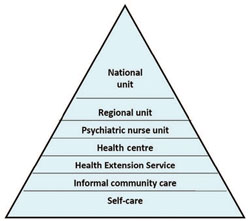
Figure 9.9 shows what mental healthcare is available for people with mental illness in Ethiopia. At the bottom, the biggest part of the triangle is labelled ‘self-care’. Self-treatment describes how the person with mental illness does things to try to help themselves, e.g. talks to someone they trust about their problems, stops drinking heavily, takes a rest from studying, and so on.
Usually when self-care isn’t enough to solve the problem, a person with mental illness will then access ‘informal community care’. This might include going to a priest or religious person for healing, e.g. holy water, driving out demons, or consult one of the traditional healers such as a herbalist, or a witch doctor (tanquaye). While a person with mental illness may find some of these healing practices to be helpful, other traditional practices may be harmful, e.g. beating, fumigation, instructing people to stop taking their medication. These harmful practices can be considered to be ‘abuse’.
As you can see, every level of the healthcare system in Ethiopia (from the Health Extension Service right up to the national referral units in Addis Ababa, e.g. Amanuel Hospital) needs to be involved in delivering mental healthcare. That is essential if we want to increase the number of people with mental illness who receive effective treatment. There aren’t enough psychiatrists and psychiatric nurses to see everybody who needs help. In any case, people with mental illness often don’t want to go to specialist mental health services. If mentally ill people can receive care from local health services then they don’t have to travel so far and they won’t have to spend so much money.
9.3 The treatment gap