4.4.3 Key HIV prevention strategies for young people that you can offer at health posts
HIV prevention services must be offered to young people whenever they come for health services (STI, antenatal care, family planning, etc). Key prevention strategies for young people cannot be the same for all but need to be adapted to their different needs. For example for boys and girls in primary school (early adolescence age 10–14), it is appropriate to talk about the changes during puberty and the benefits of abstinence and delaying sexual activity. By contrast, for post-adolescents (aged 20–24) education about faithfulness and safer sex using condoms is relevant as they are likely to have started sexual activity anyway. Similarly, you need to provide appropriate messages for adolescents in and out of school and young people both married and unmarried based on their needs for information and services.
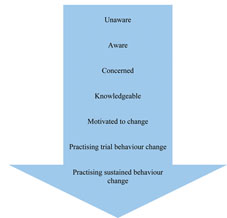
Postponing the first sexual activity and reducing the number of sexual partners can significantly protect young people from HIV. Behavioural change communication can help young people to develop positive behaviours. Behavioural change communication is the process of using communication approaches and tools to develop the skills and capabilities of individuals to promote and manage their own health and development. It promotes positive change in their behaviour, as well as in their knowledge and attitudes. The messages and the way the messages are given are very important for young people, as they do not want to only hear what they cannot do, but also what they can do. Figure 4.3 shows the stages of behaviour change that an individual passes through, from being completely unaware to making positive behaviour changes.
As you can see in Figure 4.3, behaviour change doesn’t immediately follow awareness. It takes some time for individuals to change their behaviour even after they have the necessary knowledge. Hence, whenever you counsel young people who are already engaged in some form of risky behaviours (such as having multiple sexual partners, chewing khat, or drinking alcohol), it is important that you tell them they shouldn’t expect everything to change overnight. Behaviour change is a process that needs to be continuously supported and reinforced in order to bring the desired change.
Provider-initiated testing and counselling and voluntary counselling and testing (VCT) services need to be available at all health facilities and in the community. These methods can be used both for giving information on sexual behaviour and HIV and also for opening the discussion on many sensitive issues faced by young people (e.g. peer pressure, condom negotiation, unwanted pregnancy, decision making, how to be an adult, disclosure of HIV status). There are more details on provider-initiated testing and counselling in Study Session 26 of the Communicable Diseases, Part 2 Module.
The use of latex condoms to prevent the exchange of body fluids during sex is an essential element of all HIV prevention activities. Safer sex depends on the correct and consistent use of condoms, so condom provision must be accompanied by clear instructions on condom use for every act of penetrative sex. Female condoms offer women an option that may give them more control but they also require more counselling and assistance with respect to their proper use and they are also more expensive and less available. Condom promotion also supports dual protection.
What is meant by dual protection?
Dual protection is the simultaneous protection against unwanted pregnancy and the possible transmission of STIs including HIV.
STIs greatly facilitate HIV transmission and acquisition between sexual partners, so treating and preventing them is an important step in HIV prevention. Effective and early treatment of STIs is an essential part of HIV prevention. Hence, it’s important that you refer adolescents with STIs to minimise the risk of transmission and complications.
4.4.2 Who has a role in HIV prevention?