3.1 Infection prevention and control
As a healthcare assistant you must practise in a way that keeps the risk of transferring infection to a minimum, whether from yourself to patients or between patients. Infections and infectious diseases are caused by harmful germs, also called pathogens, such as bacteria and viruses. Most pathogens are so small that they cannot be seen without a microscope, but they are all around us.
There are a number of things you must do to prevent infections from spreading:
- prepare food safely
- carry out good hand hygiene
- make sure all equipment is cleaned properly
- dispose of waste safely
- manage laundry safely
- use personal protective equipment
- don’t go into work if you have an infectious illness.
Safe food preparation
Micro-organisms can live in food, and certain raw foods will need to be cooked to remove them. Before handling and/or preparing food, you should remove jewellery and wash your hands thoroughly. Equipment should be washed in hot soapy water between uses. Ensure food is cooked thoroughly and that food stored in a fridge is labelled, dated and kept at 5°C. Raw and cooked foods should be prepared separately. Check what precautions are taken within your workplace to ensure food poses minimal risk to your patients.
Good hand hygiene
The National Institute for Health and Care Excellence (NICE) describes five points when health and social care workers should clean their hands (NICE, 2012). These are:
- immediately before every episode of direct patient contact or care, including aseptic [cleaning] procedures
- immediately after every episode of direct patient contact or care
- immediately after any exposure to body fluids
- immediately after any other activity or contact with a patient's surroundings that could potentially result in hands becoming contaminated
- immediately after removal of gloves.
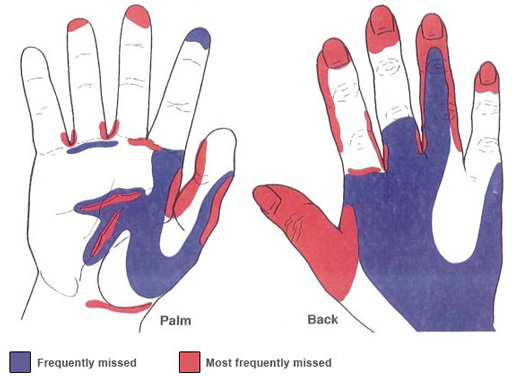
In addition, NICE (2012) defines an effective handwashing technique as involving the following three stages: ‘preparation, washing and rinsing, and drying. Preparation requires wetting hands under tepid running water before applying liquid soap or an antimicrobial preparation. The handwash solution must come into contact with all of the surfaces of the hand. The hands must be rubbed together vigorously for a minimum of 10–15 seconds, paying particular attention to the tips of the fingers, the thumbs and the areas between the fingers. Hands should be rinsed thoroughly before drying with good quality paper towels.’
When hand-washing you should remove your wristwatch and any jewellery on your hands and lower arms, and wash right up to your elbows, paying particular attention to your thumbs and the space between your fingers, areas which are commonly missed. It is also important to ensure that fingernails are clean (without nail varnish) and kept short. Remember to make use of alcohol gels supplied within your setting, and to cover any cuts you have on your hands with waterproof dressings to avoid cross-infection.
Safe disposal of waste
Clinical waste is any waste which consists of:
- human or animal tissue
- blood or other body fluids or excretions
- drugs or other pharmaceutical products
- swabs or dressings
- syringes, needles, blades (stitch removers) or other sharp instruments
Any of these could cause harm to a person coming into contact with it, and so hazardous waste must be disposed of in a way that avoids any danger or harm to yourself or other members of staff. Your workplace will have a policy about this.
Safe management of laundry
Linen that comes into contact with workers or individuals can become contaminated with harmful micro-organisms and should be washed separately from other items. Soiling is likely to include blood and tissue, sputum (a mixture of saliva and mucus), urine, vomit and faeces. Personal protective equipment (PPE) must be worn when handling infected linen as it can transfer germs to skin and clothing. Uniforms or work clothing should be changed daily and washed on a hot wash, then tumble-dried or hot ironed, to kill any bacteria present.
Correct use of personal protective equipment (PPE)
The most common PPE you will use as a healthcare assistant are disposable aprons, gloves and masks, all of which will be for single-use only. Disposable aprons protect clothing and uniforms from contamination from blood and body fluids, and you should be issued with enough uniforms for regular changing. Gloves play an important role in protecting workers from exposure to blood-borne viruses, especially where there is a risk of injury such as a puncture wound with contaminated sharps, abrasions or cuts. Masks protect you from breathing in harmful micro-organisms, and eye protection and face shields should be worn if there is a risk of being splashed with body fluids.

Activity 4
The law says that individuals should be provided with the correct materials and equipment to protect them from injury and, as far as possible, from the risk of infection while at work. If appropriate, think about occasions when you have had to wear or use PPE at work. Write down in the space below what type it was and why you had to use it.
Comment
If you already work as a healthcare assistant, there must be numerous times you’ve had to wear PPE: for example disposable aprons when bathing a patient, gloves when changing dressings and masks for surgical procedures. What does it feel like to wear PPE, and how does it make patients feel when cared for by someone wearing it?
Infectious illness
If you have cold or flu symptoms (such as coughing or runny nose), an upset stomach or skin infections, you should speak to your manager before reporting for work. If you have diarrhoea or vomiting you should not attend work until you have been free from symptoms for 48 hours.
Good hygiene is important for everybody, but as a healthcare assistant you have a duty to adopt these safe measures for your own and others’ safety.
3 Health and safety in your workplace