3 Planning ahead for older age
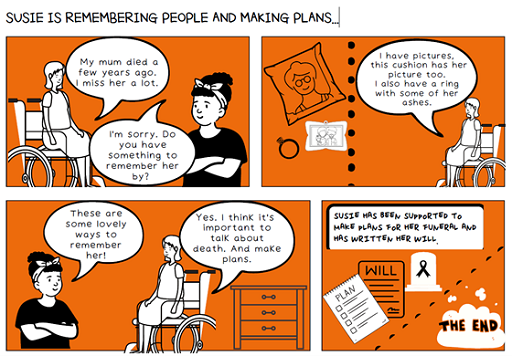
Ageing well includes holistic and coordinated planning for end-of-life care. It is about living your best life now while also thinking about writing a will and planning your funeral. While Susie is content living in the care home proactive plans are needed for the future.
The care home has developed a comprehensive guide to end-of-life care for people with learning disabilities. Every person has this plan. The plan focuses on their current health and care support needs as well as anticipating changes which may present as the person grows older. It is a holistic package of care.
Susie is 60 years old. She was born with a condition called Cerebral Palsy. It has affected Susie in a range of ways and may cause further physical and mental health difficulties as she gets older. Using their guide, the team supporting Susie can anticipate the health changes and can call on support from health professionals when required. Susie has been fully involved in thinking ahead to write a living will and plan her funeral.
Activity 3 Planning for end of life
Read the accounts from Susie’s brother and the clinical nurse lead supporting Susie as they talk about why it is now so important to get plans in place for when she gets older.
As you read, reflect on what plans, if any, you have already made for yourself or for someone you are supporting and what you might consider making.
Susie’s brother:
We in fact done a living will with her, I don’t know if you know that. Obviously, a verbal one because she can’t write or anything, in front a member of, I think it was [nurse] I think, whereby it was discussed about what we’re going to do with your money and things when you go…We also, at the same time we discussed her funeral. We’ve all got, if I’m still around, everybody’s got to wear pink, her favourite colour. And that’s stuff we’re going to do, we’ll go through and sort it out and it’s paid for it’s for any funeral, it’s all sorted out, done and dusted, paid for. The same people who took care of my mother and then her ashes will be scattered in [local] Crematorium in the very same spot my mother was. So, you know, and my father is there anyway. As I say I’m not religious but there you go. So it’s all in place and as I say she’s aware that you get older and eventually you go. Oh Yes, she certainly put her point of view across about everything don’t worry.
Clinical nurse lead:
Susie does have some more understanding and because she’s had death in the family that she’s grieved for. We were looking at getting her a funeral plan. So she had some inheritance from her mum, and we wanted to make sure she had a funeral plan ready and she at first found that really difficult because she thought we meant she were going to die, like now and that’s why we needed a funeral plan. So her brother was involved with it…I mean he said if Susie didn’t have the money, he’d pay for her funeral anyway. That it isn’t something he wouldn’t do but he just wanted to plan for the future. So we sat down, and we said to her so all we want to look at is we want to look at what kind of flowers you’d want, what kind of songs and have that kind of plan. And I think we did manage to explain it well enough for her that she understood that we didn’t say she was dying right now, but we just wanted to discuss what sort of things she wanted to happen in the future when that time comes. So I think it went well enough and she does have a funeral plan in place now and she said she wanted pink roses and things like that so.
Well she could change her mind a few times between now and whenever that may be as well. But yes, I suppose with her it’s difficult because of her mental health and the fact she does worry about things you have to be very careful about how you talk about it so that you don’t make her think oh that’s it, I’m dying, they’re planning my funeral for next week. We were like no we’re just planning it for the future. I mean we try and get funeral plans for all clients just to make it easier if they’ve got the money. Most of them have got the money to get a funeral plan so we speak to families about that and then it’s another thing families don’t have to worry about when it does get to that time.
Discussion
For Susie’s brother the focus was on Susie making plans for her estate (money and personal items) after her death, to ensure that Susie’s wishes are formally documented. He also focused on Susie making plans for her funeral to ensure her choices are reflected and that the funeral is planned and paid for.
The focus of the clinical nurse lead was also on the funeral plans, with recognition of the support Susie needed when making the plans and the anticipated emotional support Susie may require having made her plans. The clinical nurse lead identifies that Susie is experienced the death of a family member, and this experience has provided Susie with an increased understanding of death.
Susie’s brother and the clinical lead nurse were both focused on funeral plans but didn’t make explicit mention of how Susie might be involved in decisions related to her care at the end of life (e.g., treatment options, where she would like to be, whom she would like to support her). This has emerged as a key finding in the ongoing Victoria and Stuart NIHR project (led by Professor Irene Tuffrey-Wijne, Professor of Intellectual Disability and Palliative Care, Kingston University, on End-of-Life Care (EOLC) planning). Inclusive planning appears to be overwhelmingly focused on post-death/funeral arrangements/legacy. There are far fewer examples of people with learning disabilities being supported to participate in discussions about palliative care and dying. This deficit needs to be addressed.
When supporting people with learning disabilities it is important to remember that they ‘… have the right to be involved in discussions and make informed decisions about their care …’ (NICE, 2018 p. 8).
In the final video in this session, you will hear from our panel members as they discuss death, dying and planning for end-of-life.

Transcript
As you heard from the panel thinking about and talking about death and dying is difficult, for some it is a taboo subject. Ben identifies that health and care workers talk about supporting people with learning disabilities to have a ‘good life’ but there also need to talk about supporting people to have a ‘good death’. Excellent care and support involves having difficult conversations including talking about death, dying and end-of-life planning and involving the person in making decisions about their care and support.