1.2 Inflammation
Inflammation is a common response to tissue injury or infection, and occurs when the body’s defence systems are brought to the site of the damage.
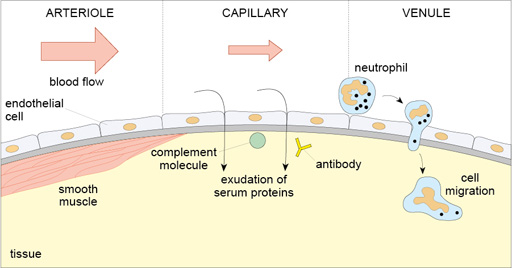
There are three main components of inflammation as illustrated in the diagram below (Figure 4).
- An increase in the blood supply to the affected area, caused by dilation of arterioles supplying the area.
- An increase in the permeability of capillaries, which allows larger serum molecules, such as antibodies, to enter the tissue.
- The migration of leukocytes from the blood into the tissues: the leukocytes cross the endothelial cells, which line the venules, and then move out into the tissue.
The blood that is brought to the site of the injury contains a number of proteins that stop bleeding, help clear infection and induce repair or regeneration of the tissues. It also contains different types of leukocyte (white blood cells) each of which have evolved to deal with different types of infection.
Inflammation can be separated into two main types.
- Acute inflammation develops quickly and resolves within days.
- Chronic inflammation can last for months or years, usually because of the persistence of the initiating factor.
More details about both types of inflammatory response, and how they can be recognised in tissue samples, is provided below.
Acute inflammation
The histological appearance of acute inflammation is quite different from that of chronic inflammation and the distinctive features can point to the initiating agent. For example, an infection of the skin with Staphylococcus aureus usually produces an acute inflammatory response, whereas infection with Mycobacterium leprae (leprosy) typically produces persistent infection and chronic inflammation.
One of the key histological differences between acute and chronic inflammation is seen in the sets of leukocytes that are present in the tissues. In acute inflammation polymorphonuclear neutrophils usually predominate, whereas macrophages and lymphocytes predominate in chronic inflammation. Eosinophils are often prevalent in sites of helminth infections (parasitic worms). Hence, the characteristics of inflammation are determined both by the tissue in which it occurs, and by the initiating agent and its persistence.
Chronic inflammation
Chronic inflammation is seen in diseases where there is persistent infection, usually because the pathogen can resist the body’s immune defences. If the infection is cleared, chronic inflammation resolves, but residual damage may still be evident in the tissues.
Chronic inflammation also occurs in many autoimmune diseases. The immune system normally recognises and tolerates all of the body’s own tissues. However, in some conditions the immune system reacts against a tissue resulting in autoimmune disease.
In autoimmunity the target of the immune response is one of the body’s own proteins or cellular components, and consequently the stimulus for inflammation cannot be cleared, although the condition may improve if the normal controls that prevent autoimmune reactions are restored. The targets may be individual molecules found in a specific tissue, or antigens present in many tissues or in the extracellular matrix.
Table 1 gives some examples of such diseases and the target antigens.
| Disease | Organ(s) | Target antigens | Histological appearance |
|---|---|---|---|
| Hashimoto’s thyroiditis | Thyroid | Thyroglobulin, Thyroid peroxisomes | Destruction of thyroid follicles with severe inflammation |
| Goodpasture’s syndrome | Kidney Lung | Basement membranes | Damage to kidney glomerulus and/or lung alveoli |
| Myasthenia gravis | Skeletal muscle | Acetyl choline receptor | Degeneration of the motor endplate at nerve/muscle junction |
| Pemphigus | Skin Mucosa | Desmosome proteins in keratinocytes | Separation of layers of epithelium |
| Type 1 diabetes | Islets of Langerhans | Pancreatic beta cells, insulin, GAD (enzyme) | Selective damage and loss of cells of pancreatic islets with inflammation |
| Multiple sclerosis | Brain Spinal cord | Components of myelin | Focal areas of inflammation and loss of myelin in the central nervous system |
Inflammation is associated with many types of tissue damage, although the appearance will vary depending on the tissue and the initiating factor. The slide collection that you will examine shortly includes some examples of inflammation as a consequence of infection.