Cancer treatments including chemotherapy, radiotherapy, targeted therapy or surgery can compromise a patient´s immune system. Therefore, the risk of becoming seriously ill with SARS-CoV-2 could be higher.
How does chemotherapy impact a cancer patient's response to COVID-19?
Many chemotherapeutic agents work by slowing the growth of rapidly dividing cancer cells. Chemotherapy is used to treat cancer (both cure or prevent recurrence) and ease cancer symptoms (used to shrink tumours that might be causing pain). However, some forms of chemotherapy can damage other healthy tissues that also divide rapidly. For example, it can kill the white blood cells that are an essential component of our immune system.
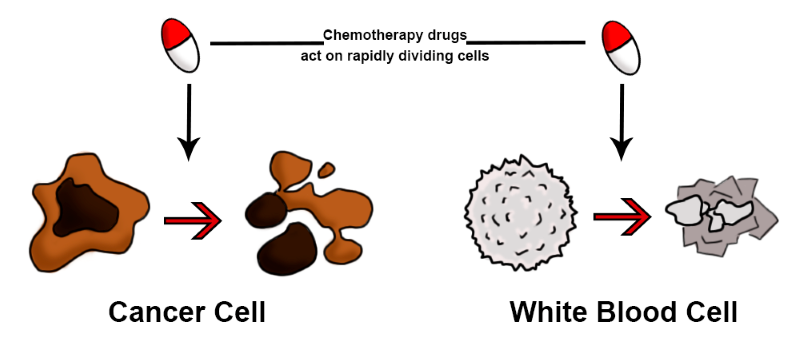 Chemotherapy targets and kills fast dividing cells such as cancer cells, but may also deplete the protective cells in the immune system such as white blood cells
Chemotherapy targets and kills fast dividing cells such as cancer cells, but may also deplete the protective cells in the immune system such as white blood cells
Reduction of white cells has the greatest impact on the immune system. When the white blood cell count is lower than normal, cancer patients are more prone to infection. A type of white blood cell known as neutrophils are especially important because they are the first responders to infection. Patients are particularly at risk of getting an infection 7 to 14 days after having chemotherapy, when the level of white blood cells is at its lowest, although this can vary depending on the drug used.
How much of an impact any given chemotherapy has on a cancer patient´s immune system depends on many factors, such as:
- Is chemotherapy being taken in combination with other drugs?
- What dose has been given and how frequently?
- How long does the treatment last?
- The cancer patient´s age, health and any additional underlying conditions
Cancer patients should rely on their doctors´ expertise to consider the benefits and risks of their chemotherapy plan. Cancer patients will be asked to self-isolate if they are undergoing chemotherapy.
A recent report showed that people receiving anti-cancer treatments (chemotherapy or surgery) in the two weeks before contracting the new coronavirus were at higher risk of dying. From the 18 patients considered, 4 of them had received chemotherapy or surgery in the past month. 3 out of those 4 patients (75%) developed severe COVID-19 symptoms. In contrast, only 6 out of the remaining 14 patients (43%), who were no treated with chemotherapy or surgery, showed severe COVID-19 symptoms. It is important to note that this data is from a small cohort of patients with COVID-19 and, although suggestive, it needs to be carefully interpreted and validated by other independent studies.
How does radiotherapy treatment affecting the immune system in relation to COVID-19?
Radiotherapy is the treatment where radiation is used to kill cancer cells and/or shrink the tumour.
There are different types of radiotherapies, the most common ones being:
- External where beams of radiation are carefully aimed at the cancer.
- Implants consist of small pieces of radioactive material that are temporarily inserted around the cancer.
- Oral administration or injections a radioactive liquid that is administrated to the patients either orally or by injection.
- Intrabeam where radiotherapy is delivered immediately after cancer surgery, typically used in breast cancer.
Radiotherapy’s impact on the immune system is usually lower than chemotherapy. However, there is still a chance that the immune system will be compromised by the radiotherapy treatment, especially if radiation is directed at the bones where the red marrow produces immune cells that enter the blood circulation. Radiotherapy uses radiation to damage cancer cells and, unfortunately, surrounding cells might be damaged as well. If cancer patients are being given a focused radiotherapy treatment that avoids the bones, it is very unlikely this will affect their immune system. However, if the cancer is located near or within the bones, the immune system could be compromised and weakened.
At the moment, there is not enough data to determine whether there is any correlation between radiotherapy treatment and COVID-19 severity. However, given the importance of the immune system to fight against viral infections, we can speculate that cancer patients undergoing radiotherapy affecting their immunity would have a higher risk of becoming severely ill with COVID-19. For this reason, patients are advised to speak to their clinician to get a blood test to determine how their specific radiotherapy treatment is affecting their immune system and to self-isolate.
If someone is undergoing targeted treatment, does that mean they are a vulnerable group for severe COVID-19?
Without large-scale scientific evidence, clinicians are forced to weigh the benefits and risks of changing cancer patients' treatment plans according to each individual´s specific needs.Targeted cancer therapies are drugs that interfere with "molecular targets" that are involved in the growth, progression, and spread of cancer. There are different types of targeted treatments, such as hormone therapy, cell signalling inhibitors, gene expression modulators, cell death inducers, or immunotherapies.
Targeted therapies are less toxic to healthy cells than chemotherapy because they are designed to target molecules that are more vital for cancer cells than healthy ones. Not all types of targeted therapy treatments will have the same impact on a cancer patient´s immune system or their response to viral infection. Therefore, it is important to speak to your doctors about the specific characteristics of the cancer treatment.
There are no reports on how targeted therapies in general might affect COVID-19 progression. However, there are some anecdotal case reports about individual patients. For example, one patient with a specific type of lung cancer that can be treated with Osimertinib (a cell signalling inhibitor therapy commonly used in this cancer) was diagnosed with COVID-19. This patient was successfully treated for SARS-CoV-2 while still being under treatment with Osimertinib. Clinicians reported no adverse outcomes for this patient. This anecdotal report illustrates that, without large-scale scientific evidence, clinicians are forced to weigh the benefits and risks of changing cancer patients´ treatment plans according to each individual´s specific needs.
Does being on hormone therapy increase the risk of COVID-19?
Hormones are a class of signalling molecules produced and released by various glands in the body that regulate the activity of cells or organs. Hormones are essential for the correct function of many bodily functions such as blood sugar levels, sleep cycles, growth and mood balance. However, the growth of some cancers is increased by specific hormones. One example is prostate cancer, where the hormone testosterone accelerates the cancer growth.
Whether a hormone treatment might increase the cancer patient's probability of becoming severely ill from COVID-19 will depend on the specific hormone treatment.Hormone therapy uses medicines to block the production and/or function of specific hormones to delay the growth of the cancer. In the case of prostate cancer, there are various medicines that block the production of testosterone. Usually, prostate cancer patients are offered hormone treatments such as anti-androgen tablets, which are considered standard hormone therapy treatments for prostate cancer and help to control the development of the cancer. If applied in combination with other cancer treatments such as radiotherapy, hormone treatments can dramatically improve the overall efficacy of the cancer treatment.
Hormone treatments have side-effects that are closely related to the function of the hormone that they target. For this reason, whether a hormone treatment might increase the cancer patient´s probability of becoming severely ill from COVID-19 will depend on the specific hormone treatment. The Healthcare team will advise patients whether their treatment has been previously reported to weaken the immune system. One example is Enzalutamide (Xtandi®), which blocks testosterone from reaching the prostate and has been also found to reduce the number of white cells in the blood, hence, compromising the immune system.
How does immunotherapy affect a person’s response to COVID-19?
Our immune system is constantly finding and removing abnormal cells that, if left undetected, could develop into a cancer. However, many cancer cells manage to switch off this immune surveillance role, making them ‘invisible’ to the immune system. Immunotherapy is a type of cancer treatment that helps the immune system rediscover and attack cancer cells.
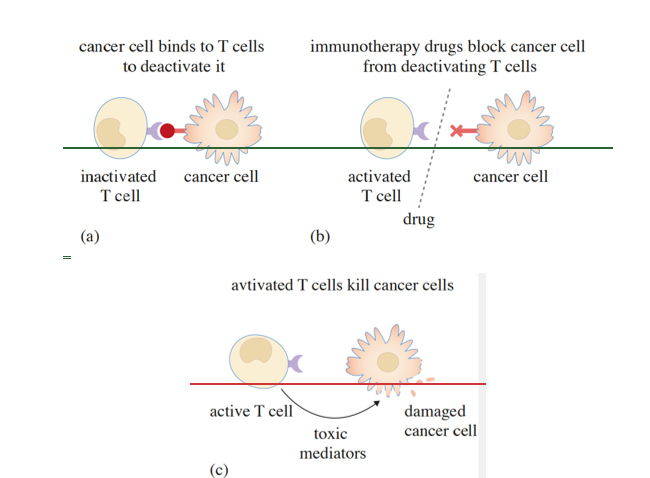 How immunotherapy works to boost the immune system via checkpoint inhibitors so that cancer cells can still be recognised and removed from the body.
How immunotherapy works to boost the immune system via checkpoint inhibitors so that cancer cells can still be recognised and removed from the body.
This therapy relies on boosting the immune system response against the cancer cells mirroring how we would fight an infection. There are different types of immunotherapy approaches, which include:
- Immune checkpoint inhibitors which overcome the way cancer cells block the immune response.
- T cell transfer therapy consists of collecting specific immune cells from a patient’s blood (called T cells) and genetically modifying them so they can recognise proteins expressed on cancer cells. They are then transplanted back to the patient in order to boost the immune response against the cancer.
- Monoclonal antibodies are immune system molecules that attach to cancer cells and increase their visibility to the immune system.
- Cancer vaccines work by boosting the immune system against cancer cells.
- Immune system modulators use of specific agents that are part of the immune response to improve the reaction against cancer cells.
Some immunotherapies might decrease the total number of white cells in the blood and could potentially increase the risk of COVID-19 infection. For this reason, it is very important to consult with healthcare teams to understand the specific risks of each individual treatment.
Immune system modulators include cytokines, which are proteins normally made by the white blood cells that are vital to our early ability to detect and destroy cells infected with viruses. Unfortunately, some side effects of cytokine treatment include lowering the total number of white cells. This is the case with interferon gamma (IFNy), which is commonly used in kidney cancer, multiple myeloma or some types of leukaemia to boost the immune system response. In fact, white cell counts typically decrease by 30–50% during IFNy therapy.
Regarding the relationship between immunotherapy and COVID-19, no clear data are yet available. There is an anecdotal case report from an Italian patient who suffered from metastatic lung cancer and was being treated with Nivoumab (a drug that prevents cancer cells from evading the immune system) for the last 7 years. The patient died with COVID-19 rapidly from the first sign of symptoms. It is impossible to conclude whether the immunotherapy treatment affected this patient´s outcome for COVID-19. However, it emphasises the fact clinicians will weigh the best approach for their patients and that more research is needed to understand the relative COVID-19 risk of patients exposed to different immunotherapies.
Stem cell transplant and COVID-19
Blood forming cells in the bone marrow can become depleted by radiotherapy or chemotherapy. Stem cell transplants are used to restore blood-forming stem cells. After a stem cell transplant, patients are more at risk of becoming seriously ill from COVID-19 because it can take a while for the immune system to return to full strength.
If a cancer patient has received stem cells from a donor, they are usually asked to take medicines that stop their immune system from working so strongly (immunosuppressants), to reduce the risk of their body attacking the transplanted cells, or to reduce the risk of the transplanted cells attacking other cells in their body. Patients taking immunosuppressive drugs are at particularly high risk of serious COVID-19 infection and are therefore included in the “vulnerable people” group by the UK Government.
In this series of articles we explore how COVID-19 impacts on cancer patients and their treatment. Read on to discover the frequently asked questions relating to COVID-19 and cancer ...




Rate and Review
Rate this article
Review this article
Log into OpenLearn to leave reviews and join in the conversation.
Article reviews