3 Assisted dying
Assisted dying is currently not a feature of end-of-life care policy in the UK. The assisted dying debate is one that continues to divide opinions and is now regularly debated within the courts and parliaments. In countries that do allow it, it is offered alongside palliative and end-of-life care (e.g. the Netherlands).

Some people argue that if end-of-life care was better, people would then not want assisted dying because their pain and other symptoms, including psychological and social, would be managed. Others argue that even with such holistic care, some individuals may wish to choose when and how they die. However, research suggests that requests for assisted dying or euthanasia actually increase among people receiving hospice (i.e. end-of-life) care (Chapple et al., 2006; Lawton, 2000; Seale and Addington-Hall, 1995). A number of reasons for this have been suggested, including the greater openness of expression encouraged in hospices, the distress of witnessing other people’s deaths and wanting to avoid a similar experience, and the wish to remain physically independent and ‘in control’ (Chapple et al., 2006). In countries where assisted dying is legal, there is some evidence to suggest that not everyone who requests assisted dying follows through with the act (Warnes, 2014).
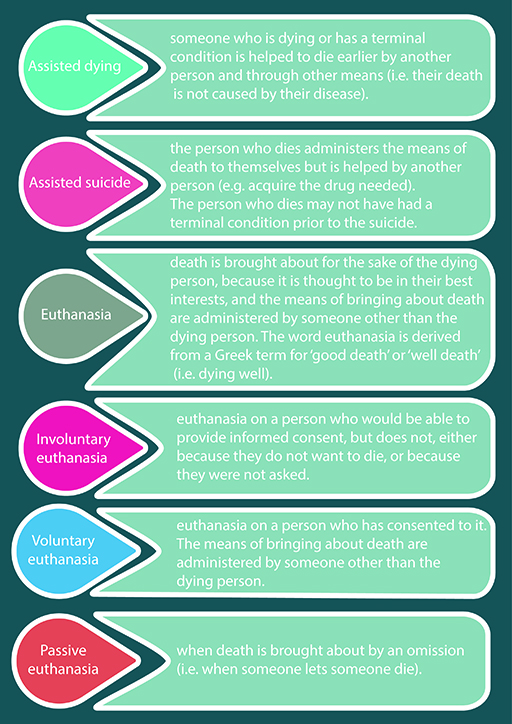
Before you look into the reasons for and against assisted dying in more detail, it is useful to understand the range of terminology that is used within this topic. As with end-of-life care, there are several terms used to describe a range of subtle differences. This is explained in Figure 8.
Note how there are differences in these terms about who does the action, the intention of the action, and if the person who dies had a choice about the matter. In the media, there are often debates around legalising assisted dying. For example, assisted dying may be seen to some as more ethically defensible than prolonging a slow or painful death. Also some believe that it is an individual’s right to choose their death (personal autonomy) and achieve the death that they want at a time that they want which might allow them to have a dignified death (Rodgers, Booth, Norman, & Sowden, 2016). The debate about the right to die is often covered in the news media, such as when Paul Lamb (who was a paralysed former builder) and Jane Nicklinson (a widow of a man who had locked-in syndrome) lost their legal fight to allow disabled people the right to die. This issue was covered and reported in the news (ITV News. Hope remains despite Supreme Court rejection of right to die campaign, 2014). In the entertainment media, the UK TV drama Coronation Street has also included a storyline in which a long-standing character, Hayley Cropper, die in an assisted suicide (ITV News, Coronation Street shows controversial right to die scene, 2014).
In the next activity, you will be asked to watch a video featuring Actress and Activist Liz Carr who is speaking against legalising assisted dying.
Activity 3 A case against legalising assisted dying
Watch this video featuring British actress Liz Carr describe why she opposes legalising assisted dying:

Transcript: Video 4
[TEXT ON SCREEN: Liz Carr talks to Tasmania about Euthanasia]
Make a few notes about what problems or issues Liz Carr thinks that legalising assisted dying might raise.
Discussion
Liz Carr argues that there is often a fine line between what people consider terminal illness and disability and that legalising forms of assisted dying may mean that people who are disabled may inadvertently be subject to subtle or direct coercion. Liz raises many points, including how there is no evidence to assure vulnerable people (older and disabled people) that their voices will be heard if assisted dying was legal. There is little or no evidence about how this is done successfully in places which have already legalised some forms of assisted dying. Liz highlights that assisted dying offers benefit for the few but is a risk to many (vulnerable) people. Liz also explains that in the cases of physician-assisted deaths, it is often the same doctors who assess the patient, who will carry out and evaluate whether the death was a good death – which doesn’t allow for much oversight. You may have written down other points.
If you have been affected by the issues in these videos, you can call Macmillan Cancer Support [Tip: hold Ctrl and click a link to open it in a new tab. (Hide tip)] free of charge on 0808 808 00 00. You can also call Samaritans free from any phone on 116 123 (it will not appear on your phone bill), email jo@samaritans.org, or visit www.samaritans.org to find details of your nearest branch. The Motor Neurone Disease Association also provides support to people affected by motor neurone disease in England, Wales and NI - 03457 626262 or visit The Motor Neurone Disease Association