27.1 Transmission of HIV from mother to child
We know that not every baby born to an HIV-positive mother will be infected by the virus. This is because the placental membrane between the fetus and the mother remains intact during pregnancy.
The placental membrane forms a barrier between the blood of the mother and the fetus, limiting the transmission of HIV.
However, if the HIV-infected mother has problems during pregnancy, such as a lack of antenatal care (ANC), infections or poor nutritional support, she may become sick, which will further weaken her immunity. As a consequence, the number of viruses circulating in her blood will rise, and this increases the likelihood of the virus crossing the placenta and infecting the unborn child.
HIV is mostly transmitted from mother to child during delivery, at a time when the cuts and abrasions that often occur during birth increase the risk of the baby coming in contact with his or her mother’s blood. Therefore, it is essential that an HIV-infected pregnant woman is supported by ANC services, and that she delivers her baby safely at a health facility, as illustrated in Figure 27.1. Importantly, if the baby is born in a setting where birth trauma is less likely to occur, the likelihood of transmission of HIV from mother to child is reduced.
It is part of your role as a Health Extension Practitioner to counsel and encourage a pregnant mother to come to you for antenatal care, and to give birth to her baby at a health facility.

After delivery, HIV may be transmitted from mother to child through breastfeeding (although the risk is not as high as that during delivery). During breastfeeding, the virus may pass through the gut wall of the baby, particularly if it is inflamed, due to infection, by bacteria causing diarrhoea.
PMTCT can reduce the chances of HIV from mother to child from 30% to 10%. This is a dramatic improvement, and HIV-positive mothers should be encouraged to seek PMTCT.
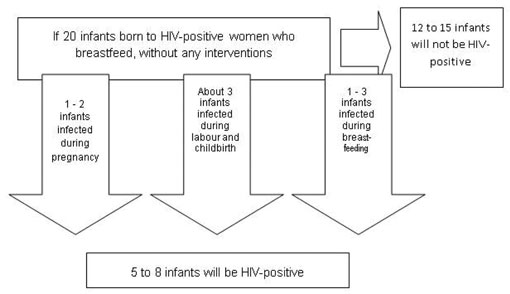
The risk of HIV transmission from mother to child for pregnant women who are not supported by ANC and PMTCT services is summarised in Figure 27.2. It has been estimated that 30 out of 100 babies (30%) born to mothers with HIV will be infected with the virus if the mothers do not attend ANC to receive PMTCT services. The outcome can be dramatically improved if the HIV-infected mother takes prophylactic drugs, which greatly reduce the chances of her baby becoming infected with HIV. The success of chemoprophylaxis depends on the drugs taken, and on good antenatal care follow-up to ensure adherence to treatment. In general, less than 10 out of 100 children will be infected by HIV if drugs for PMTCT are taken by the mother.
Learning Outcomes for Study Session 27