30.2.1 Management of pain in PLHIV
Pain is one of the most common symptoms in HIV/AIDS patients with advancing disease. If your patients complain of pain, they should be assessed carefully (as described below); severe cases should receive urgent referral for specialist consultation and treatment.
How to assess pain
First, ask the patient ‘Where is the pain?’ and ‘What makes it better or worse?’ ‘What type of pain is it, and what medication (if any) is being taken for the pain?’ Note that pain could result from severe opportunistic infections, and this may need urgent referral to a health centre or hospital.
Secondly, determine the type of pain. Is it a familiar pain (such as bone or mouth pain), or a special and unusual pain (such as shooting nerve pain or muscle spasms)?
Thirdly, check if there is a psychological or spiritual component to the pain. Does it feel worse when the patient is depressed or anxious? Does it feel better when the person is doing something interesting that takes their attention away from the pain?
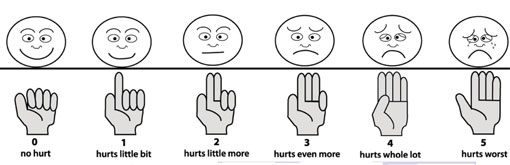
Fourthly, grade the pain from 0 to 5 with the faces chart (especially when working with children), as illustrated in Figure 30.1, or using your hand with different numbers of fingers raised (no fingers being no pain, and five fingers the worst possible pain).
How to manage pain at community level
Manage the pain with paracetamol if it is at grade 1 or grade 2. Paracetamol is the anti-pain medication that you are allowed to give at community level. Refer patients with pain at grades 3, 4 and 5 to the nearest health facility.
Why do you think you should refer patients with grade 3 pain or above?
You should refer such patients quickly because the pain may be indicating severe disease, which needs better diagnosis and management with anti-pain drugs that can only be given by a doctor.
Pain can also be managed without the use of modern medication. Indeed, spiritual and emotional support and counselling should always accompany pain medication. This is because pain can be harder to bear when there is guilt, fear of dying, loneliness, anxiety or depression. Likewise, answering questions and providing information on HIV/AIDS health-related issues is important to relieve fear and anxiety, which in turn makes pain more bearable. The other ways to relieve pain are deep breathing and relaxation techniques (unless the patient has severe mental health problems); or distracting the patient’s attention using music, conversation, or imagining a calm scene.
In your catchment area, how do people treat pain without using modern medication? Give two examples of local pain treatments which are not effective in relieving chronic pain.
Local pain remedies vary in different parts of the country, but you may have thought of tying the painful area with a scarf or other cloth to treat headache or back pain; or burning the skin of the painful area using very hot wooden or metal sticks, sometimes to treat headaches, but mainly for pains in the hands and feet. These treatments are not effective and can make the pain worse. Burning the skin creates a wound that could become infected.
 Traditional medication for pain relief may interfere with ARV drugs. Refer patients to the nearest health centre for advice on this topic.
Traditional medication for pain relief may interfere with ARV drugs. Refer patients to the nearest health centre for advice on this topic.
30.2 Symptom management, including pain management
