34.1.1 Amoebiasis
Amoebiasis is a disease resulting from infection of the large intestine (colon) by a protozoan parasite called Entamoeba histolytica.
The distribution of this single-celled parasite is very widespread – the WHO estimates that around 500 million people around the world are infected with these amoebae (Figure 34.1). It is endemic in Ethiopia, and research studies have shown a prevalence of amoeba infection ranging from 4% to 19% in the Ethiopian population.
However, most people with amoebae in their intestines show no symptoms, but they can pass on the amoebae to others and are an important reservoir of infection. Individuals who develop amoebiasis (the plural amoebae is pronounced ‘amm-ee-bee’), experience bloody diarrhoea (so the disease is also known as ameobic dysentery), fever and abdominal cramps, sometimes alternating with periods of constipation. Unlike in cases of bacillary dysentery, the blood and mucus is mixed with solid stool and patients are not usually bedridden. Very rarely, amoebiasis can lead to serious complications, including abscesses in the liver, lungs or brain.
Another difference between dysentery caused by ameobae and dysentery caused by Shigella bacteria is that amoebiasis mainly affects young adults; it rarely occurs below the age of five years. By contrast, dysentery in children under ten years is mainly due to Shigella species. Also, amoebiasis does not usually produce epidemics, so an epidemic of dysentery is most probably due to cases of shigellosis.
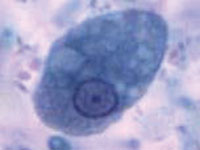
Some amoebae in an infected person’s intestines transform and become encased in a round protective membrane called a cyst. The cysts pass out of the body in the faeces. They are highly resistant to damage and can be transmitted by direct and indirect faeco-oral routes, mainly via contaminated food or water. They hatch out in the new person and the protozoa rapidly increase in number by cell division.
For accurate diagnosis, laboratory identification of the cysts in the patient’s stool is necessary to differentiate it from shigellosis. Therefore, you should start any patient with dysentery on rehydration with ORS and refer them to the nearest higher level health facility for further investigation and specialist treatment. Advise the patient or caregiver that further investigation is needed for diagnosis and that early treatment is important because the disease could lead to serious outcomes.
34.1 Intestinal protozoal diseases
