39.1.4 Clinical manifestations of trachoma and disease progression
![]() Wash your hands thoroughly with soap and water before and after each eye examination!
Wash your hands thoroughly with soap and water before and after each eye examination!
As a Health Extension Practitioner you should examine affected children and adults to identify the severity of the trachoma. Use your clean hands and a pen to turn the eyelids upwards, so you can see the conjunctiva, as illustrated in Figure 39.3.

The clinical manifestations of trachoma have been classified by the World Health Organization (WHO) into five grades indicating how far the disease has progressed. The first grade is the earliest manifestation of the infection, and the fifth grade is permanent eye damage causing sight loss and leading eventually to blindness. It is important for you to know the signs that indicate these grades, because the actions you take when you see a person with suspected trachoma depends on correct grading. The names and code letters of the five grades are given in Box 39.1; they are each described in detail below the box.
Box 39.1 The five grades of trachoma progression
First grade = Trachomatous follicles (TF)
Second grade = Trachomatous inflammation (TI) or (TF+TI)
Third grade = Trachomatous scarring (TS)
Fourth grade = Trachomatous trichiasis (TT)
Fifth grade = Corneal opacity (CO)
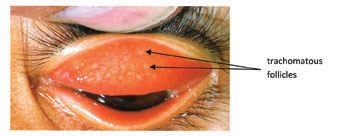
Trachomatous follicles (TF)
The first and earliest trachoma grade is characterised by the presence of five or more trachomatous follicles in the conjunctiva inside the upper eyelid. They are round, slightly raised, whitish areas of at least 0.5 mm in size (Figure 39.4). Trachomatous follicles should not be confused with trachoma scars, which are flat (see Figure 39.5 below), or the normal eyelash follicles on the edge of the eyelids. Other signs that you may notice are redness and swelling of the conjunctiva as a result of inflammation caused by the bacterial infection.
Trachomatous inflammation (TF+TI)
The second grade is when profound inflammation occurs in more than half of the upper conjuctiva, which is red, thick and swollen, and has many trachomatous follicles (Figure 39.5). In severe cases, the blood vessels of the eyelids may not be visible due to the swelling of the conjunctiva.

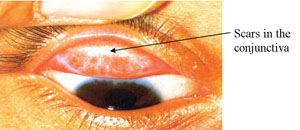
Trachomatous scarring (TS)
In time, the inflammation resolves and the follicles are replaced by scars on the conjunctiva, which appear as small glistening lines or stars, and later may become flat, thick, white bands (Figure 39.6). This is the characteristic third grade of trachoma progression.
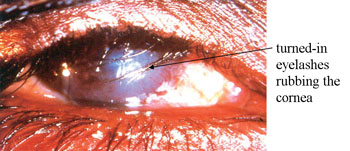
Trachomatous trichiasis (TT)
The scars gradually cause the eyelashes to turn inwards, and at least one eyelash rubs on the cornea. This sign is called trichiasis (pronounced ‘trik-eye-assis’) and is the fourth grade of trachoma severity. You can see in Figure 39.7 that many of the eyelashes are turned inwards and rub the cornea when the person blinks. This is painful and distressing for the person and it gradually damages the cornea.
Corneal opacity (CO)
A healthy cornea appears black where it covers the lens at the front of the eye. In the fifth and most severe grade of trachoma, the cornea becomes white and opaque (not transparent) as in Figure 39.8. This is known as corneal opacity.
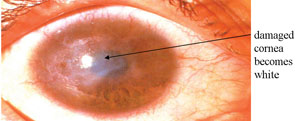
What effect will corneal opacity have on the person’s sight?
Light cannot pass easily through the opaque cornea, so the person’s sight will be severely impaired and total blindness may result.
How can you tell the difference between trachomatous follicles and trachomatous scars in the conjunctiva?
Follicles are raised and round and at least 0.5 mm in diameter. Scars are lines or bands and are flat.
39.1.3 How common is trachoma in Ethiopia?
