4.2 Intact killed pathogens
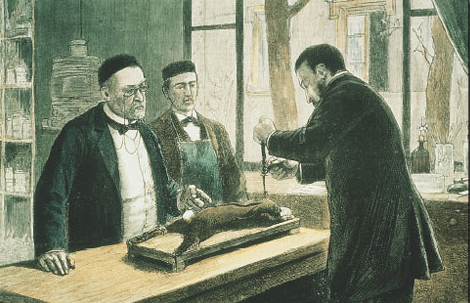
The first deliberate attempts to create a killed vaccine were made by Louis Pasteur in 1885 (Figure 4). He took samples of brain and spinal cord from rabies-infected rabbits and inactivated the (then unknown) infective agent by drying the preparation, or by chemical treatment with formalin. Although many of Pasteur's vaccines were successful in inducing protective immunity, the methods of preparation often generated vaccines with unacceptably high levels of adverse reactions. For example, the rabies vaccine sometimes induced an autoimmune reaction in the central nervous system (CNS) of immunised subjects. The vaccine included molecules from the rabbit CNS, which led to a breakdown in some of its recipients of the normal tolerance to self-molecules found in the CNS. This occurred in only a small proportion of those immunised, but nevertheless the consequences could be fatal.
Many safe killed vaccines have since been produced using chemically inactivated or heat-killed pathogens, but effectiveness is highly variable. For example, the Salk vaccine (IPV) contains an inactivated preparation of the polio virus, which elicits a strong IgG response and long-lasting protection against paralytic polio; by comparison, killed Vibrio cholerae vaccines have generally produced limited immunity for a much shorter period (see the Polio and Cholera Case Studies).
Click to view the Cholera Case Study [Tip: hold Ctrl and click a link to open it in a new tab. (Hide tip)] .
Activity 10
Both the Salk vaccine against polio and killed whole-cell cholera vaccines induce high levels of IgG antibodies. Why are IgG antibodies less useful against cholera than against polio?
Answer
Polio virus must travel from the gut through the blood to the spinal cord before it can cause paralysis. Since IgG antibodies are the principal serum antibody, they can intercept the virus as it moves from one tissue to the other. In contrast, cholera produces its damage by attaching to cells in the gut epithelium, sometimes invading them, and by the release of enterotoxin. So IgG is of limited value in defence against cholera (IgA is much more important).
